Don't miss our updates

The seminal tract is the path that sperm take from the testes to the outside. If an infection occurs at any point along this route, the inflamed areas can damage semen quality and make it harder for the egg to be fertilized. The good news is that most of these infections respond very well to antibiotics. If semen quality remains low after treatment, in vitro fertilization with ICSI is usually the best option to achieve pregnancy. What are seminal infections and how do they affect your fertility? Seminal infections arise when bacteria, fungi, or viruses reach the prostate, seminal vesicles, epididymis, or vas deferens. This can cause: Obstruction of seminal flow, causing azoospermia (absence of sperm) or oligozoospermia (fewer than 15 million/mL). Reduced sperm motility (asthenozoospermia). Abnormal sperm morphology (teratozoospermia). Increased sperm DNA fragmentation, making implantation more difficult. Production of antibodies against sperm. Possible transmission of the infection to your partner. What are the symptoms? They are often silent and only detected through a fertility study, but sometimes they present with: Changes in semen color or consistency. Irritation, itching, or burning when urinating. Urethral discharge. Discomfort in the perineal or testicular area. Avoid self-medication. If you notice any of these symptoms, stop sexual activity and consult an assisted reproduction specialist. Why do they occur? The most common causes are sexually transmitted bacteria (Chlamydia trachomatis, Neisseria gonorrhoeae) or intestinal flora (such as Escherichia coli or Enterococcus faecalis). The risk is higher with unprotected sex or multiple partners. Factors that increase the likelihood: Poor genital hygiene. Invasive urological procedures. Weakened immune system. How is it diagnosed? The specialist usually: Takes your medical history and performs a physical exam. Performs a urine culture and semen culture with antibiotic sensitivity. Orders molecular tests (PCR). Analyzes the semen with a semen analysis and DNA fragmentation test. With this information, a personalized treatment plan is designed and follow-up studies are performed to confirm that the infection has cleared. Treatment and options for achieving pregnancy Initial treatment is usually oral antibiotics for 7–14 days. It is essential that both you and your partner complete the course and maintain sexual abstinence during the medication period. Once the infection is eradicated, sperm quality is reassessed. If problems persist (concentration < 15 M/mL, motility < 40%, or high fragmentation), IVF+ICSI or additional tests in our fertility laboratory are considered. Frequently Asked Questions 1. Do they always cause infertility? No. Many are detected and treated in time, restoring semen quality. However, if inflammation becomes chronic, it can cause scarring and blockages, leading to persistent oligozoospermia or asthenozoospermia. Consult as soon as you notice any symptoms. 2. Can I infect my partner during treatment? Yes, which is why both partners should be treated simultaneously. Abstinence and condom use after therapy help prevent reinfection. 3. How does DNA fragmentation affect things? If it exceeds 30%, it can hinder natural fertilization and increase the risk of miscarriage. In those cases, ICSI along with prior antioxidant supplements is recommended. 4. Can they be prevented? With safe sexual practices (condom use), good genital hygiene, and regular check-ups if you have risk factors. A healthy lifestyle (balanced diet, exercise, no smoking) also strengthens your immune system. Sources National Library of Medicine. (2023). Male reproductive system infections. MedlinePlus. https://medlineplus.gov World Health Organization. (2021). WHO laboratory manual for the examination and processing of human semen (6th ed.). Geneva: WHO Press. Dohle, G. R., Diemer, T., Kopa, Z. (2019). EAU Guidelines on Male Infertility. European Urology, 76(4), 616–628. https://doi.org/10.1016/j.eururo.2019.08.029 Esteves, S. C., Agarwal, A. (2020). Role of oxidative stress in male infertility. Clinics, 75, e1909. https://doi.org/10.6061/clinics/2020/e1909 Remember that each case is unique. If you are looking to start a family, do not hesitate to consult an assisted reproduction specialist: we are here to support you every step of the way.
On the journey to motherhood or fatherhood, every step matters. Every hope, every dream, and every challenge brings us closer to the moment when our desire to conceive becomes reality. But sometimes unexpected obstacles arise, such as chlamydia, a silent infection that can affect our fertility. It is essential to understand how chlamydia can interfere with our plans and how we can face it with courage. Chlamydia, often surrounded by stigma and shame, can make conception difficult. However, let’s focus on our strengths and take charge of our sexual and reproductive health. Below we will see how we can protect ourselves, diagnose, and treat this infection to pave the way toward our longed-for goal: starting a family. What is chlamydia and how does it affect fertility? Chlamydia is one of the most common sexually transmitted infections (STIs) and often goes unnoticed. Caused by the intracellular bacterium Chlamydia trachomatis, it is three times more frequent in women than in men. According to the Centers for Disease Control and Prevention (CDC), around 2.8 million cases are reported each year in the U.S. In 40% of untreated cases, the infection rises from the cervical canal to the ovaries, fallopian tubes, or uterus, causing pelvic inflammatory disease (PID) or tubal blockage. It can impede fertility in several ways: Cervical infection: hinders sperm passage. Ovarian infection: alters ovulation, reduces ovarian reserve, or forms abscesses. Fallopian tube infection: causes hydrosalpinx (fluid accumulation) and increases the risk of ectopic pregnancy. Endometritis: inflames the endometrium and hinders embryo implantation. Inflammatory adhesions: obstruct the transport of oocytes and sperm. Pain during intercourse: may lead to avoiding sex on the days of highest fertility. During pregnancy, untreated chlamydia can cause: Ectopic pregnancy Spontaneous abortion Amniotic fluid infection Premature membrane rupture Preterm birth Low birth weight Neonatal pneumonia or conjunctivitis Main symptoms of chlamydia Chlamydia is often “silent”: up to 75% of infected women show no symptoms. When they appear (1–3 weeks after exposure), they may include: Abnormal vaginal discharge Burning or discomfort when urinating Bleeding between periods Pain during intercourse (dyspareunia) Pelvic pain or fever Infertility If you notice any of these signs, avoid intercourse and see a doctor as soon as possible. Early diagnosis prevents PID and greater damage to your fertility. How is chlamydia diagnosed? Diagnosis includes reviewing medical history, a brief pelvic exam, and collecting a cervical or vaginal sample for nucleic acid amplification testing (NAAT). Urine or blood tests can also detect antibodies. The CDC recommends annual chlamydia screening for sexually active individuals under 25 and for older women with risk factors. Pregnant women should be tested routinely. Since chlamydia and gonorrhea often coexist, it is advisable to test for both. In advanced cases, a transvaginal ultrasound may be necessary to assess pelvic damage. If I test positive and want to conceive, what should I do? If you test positive, abstain from intercourse until you and your partner(s) complete treatment and receive negative follow-up tests. Reinfection is common if only one person is treated. If there is tubal damage, in vitro fertilization (IVF) is the best option, as it bypasses damaged tubes. It is vital to treat the infection before starting an IVF cycle to improve success rates. Do not self-medicate; before taking any drugs, consult a reproductive specialist for proper guidance. Treatment options First-line treatment is azithromycin 1 g in a single dose or doxycycline 100 mg every 12 h for 7 days. Sexual partners must be treated simultaneously to avoid reinfection. Follow-up testing at 3 months is recommended to confirm eradication. If PID has developed, hospitalization and intravenous antibiotics may be necessary. After treatment, a fertility evaluation will guide next steps. How to prevent future infections Always use condoms, limit the number of partners, get regular tests, and maintain open communication with your partner. Routine gynecological visits help detect and treat infections early. Related resources More information at Positive Chlamydia: Symptoms, Causes and Diagnosis. Frequently asked questions 1. Can chlamydia clear up on its own? Some mild cases may resolve without treatment, but relying on this is risky. Without antibiotics, the infection can ascend, cause PID, damage the tubes, and increase the risk of infertility and transmission to your partner or baby. Treatment is the only safe way to eradicate it. 2. How long should I wait after treatment before trying to conceive? After completing medication, wait at least 7 days before resuming sexual activity. A test of cure is recommended at 3 months or sooner if symptoms recur. For IVF, confirm eradication before the cycle; your specialist will advise based on your reproductive health. 3. Does chlamydia affect ovarian reserve? Inflammation from chlamydia can reduce ovarian reserve or disrupt ovulation. While the direct link needs more study, you can assess your reserve with antimüllerian hormone (AMH) testing and antral follicle count via ultrasound. Speak to your reproductive endocrinologist if you have a history of chlamydia. 4. Is it safe to undergo IVF after a chlamydia infection? Yes, IVF is safe and recommended if there is tubal damage. Treating the infection beforehand protects the uterus and improves implantation. Your specialist may perform imaging studies and possibly give antibiotics around the transfer to minimize risks. References Centers for Disease Control and Prevention. (2023). Sexually Transmitted Disease Surveillance. https://www.cdc.gov/std/statistics/2023/default.htm Workowski, K. A., & Bolan, G. A. (2015). Sexually Transmitted Diseases Treatment Guidelines, 2015. Clinical Infectious Diseases, 61(8), e1–e42. https://doi.org/10.1093/cid/civ784 MedlinePlus. (2023). Chlamydia. https://medlineplus.gov/chlamydia.html World Health Organization. (2016). Global health sector strategy on sexually transmitted infections 2016–2021. https://www.who.int/reproductivehealth/publications/rtis/ghss-stis/en/ We are with you on this journey: having children is a deep and achievable desire. Do not hesitate to seek help from a fertilization specialist for the support and guidance you deserve.

When we talk about fertility treatments, we often think of the medical and scientific solutions that allow couples and single individuals to fulfill their dream of having a baby. But we understand that the journey also has a very strong emotional component. At Ingenes we know that taking care of your emotional health is essential for the treatment to work, which is why we offer specialized services to support you at every stage. What is emotional health and why is it key in fertility? Emotional health is the balance that helps us manage stress, anxiety, and doubts that arise during the reproductive process. With hormones, procedures, and constant appointments, it’s normal to experience ups and downs. Staying balanced not only improves your well-being but can also enhance hormone production and uterine receptivity. Do not self-medicate without consulting your doctor. If you want to increase your chances of pregnancy, always see a specialist in Assisted Reproduction. Emotional support services at Ingenes Our comprehensive program complements your treatment with: Individual and couple therapy: 50–60 minute sessions with psychologists expert in assisted reproduction to manage stress. Support groups: Weekly meetings to share experiences and feel accompanied. Workshops and talks: 90-minute activities on coping techniques, menstrual cycle, and emotional preparation. Mindfulness and relaxation: Breathing exercises, guided meditation, and adapted yoga, with daily practices of 15–20 minutes. Impact of emotional support on outcomes Chronic stress raises cortisol and disrupts the hypothalamic-pituitary axis, affecting ovulation and sperm quality. Having emotional support in assisted reproduction reduces these effects and creates a more favorable environment for implantation. Moreover, emotional backing strengthens your motivation and commitment to the treatment, improving coordination with your medical team and optimizing ovarian stimulation protocols. Additional benefits of emotional care Less anxiety: Techniques to calm heart rate and relax muscles. Better physical health: A positive emotional state improves sleep and recovery. Stronger relationship: Open communication and conflict resolution. Greater resilience: Facing setbacks with hope and a proactive attitude. Complement your well-being with the importance of nutrition in fertility treatment, where you’ll find dietary guides that support your hormonal and emotional balance. Frequently Asked Questions Can anxiety reduce my chances of pregnancy? Yes. High cortisol interferes with gonadotropin production, which is essential for ovulation and spermatogenesis. Practicing diaphragmatic breathing for 10 minutes a day helps normalize levels. Also, sleeping 7–8 hours daily is crucial for recovery and immune function. How do I choose the right therapist? Choose psychologists certified in perinatal psychology or reproductive mental health with experience in IVF or ICSI. Look for reviews from other patients and a trial session to ensure you feel comfortable and supported. When should I join a support group? From the start of your treatment you can benefit from sharing experiences. If you feel emotional fatigue, persistent sadness, or guilt, joining a group will help you express your fears and receive support. Online or in-person support? Online support offers flexibility, but in-person therapy facilitates emotional connection. Combining both formats enhances results. If you’re far from a center, schedule regular virtual sessions and at least one in-person consultation at the beginning. Sources Consulted American Society for Reproductive Medicine. (2022). Stress and Reproductive Health. Fertility and Sterility. MedlinePlus. (2023). Anxiety Disorders. U.S. National Library of Medicine. World Health Organization. (2023). Mental Health in Reproductive Care. WHO Fact Sheets. National Institutes of Health. (2021). Mindfulness-Based Interventions for Stress Reduction in Infertility. Journal of Psychosomatic Obstetrics & Gynecology. Remember: you are not alone on this journey. Taking care of your emotional health is as important as medical treatment. If you need it, see a fertility specialist for the comprehensive care you deserve. We are with you!

Our commitment to changing lives in the United States remains stronger than ever. That’s why we are proud to announce two key additions to our medical teams in San Diego and Orange County, California. These two professionals reflect Ingenes’ mission: for nearly twenty years, we have helped thousands of couples and individuals achieve the dream of having a baby. The importance of a multidisciplinary team At Ingenes, we believe every journey to motherhood or fatherhood is unique. That’s why we have a multidisciplinary, empathetic, and highly trained team. Today we welcome Dr. Miguel Marrero and Dr. José María Alanis, both with backgrounds in chemical engineering, lab protocols ranging from µL to mL, and years of clinical practice. Their expertise strengthens our San Diego and Orange County centers to support you every step of the way. Dr. Miguel Marrero in Orange County Dr. Marrero joins us from AltaMed Medical Group in Santa Ana, CA. He earned his medical degree from Case Western Reserve University School of Medicine, completed residency at Indiana University Medical Center, and internship at NYU Medical Center. He finished a fellowship in reproductive endocrinology and infertility at the Mayo Clinic, and has led labs where every µL matters for IVF protocols. Board-certified by the American Board of Obstetrics and Gynecology, he brings scientific rigor and human warmth. Dr. José María Alanis in San Diego Dr. Alanis-Amezcua studied Biological Sciences and Surgery at the UNAM, with residencies at the University of Chicago and University of Illinois Metro Group Hospitals. His fellowship in gynecologic oncology at Memorial Sloan Kettering enhances his reproductive focus. With over 20 years of practice in San Diego and La Jolla, where he handles mg doses and high-precision imaging, he is certified by the American Board of Obstetricians and Gynecologists and is a member of the American College of Obstetricians and Gynecologists. Working together as a team With the arrival of Dr. Marrero and Dr. Alanis, we reinforce our U.S. network, offering top-quality fertility services. We use standardized protocols in Mexico and the United States, coordinating every detail between Ingenes Mexico and Ingenes USA and Ingenes San Diego to shorten your path to success. Ingenes is here for you: we provide cutting-edge assisted reproduction care, with physicians dedicated to your dream of having a baby. Avoid self-medicating and, before taking any medication, consult an assisted reproduction specialist. Let’s walk together toward the parenthood you dream of! Frequently Asked Questions What should I expect at my first consultation? We review your history, hormone tests (ng/mL), and ultrasound to design a personalized plan. You’ll meet your physician, who will explain IU dosing, scheduling, and lifestyle recommendations so you feel informed and confident. How does Ingenes achieve high IVF success rates? We combine embryo culture in incubators with 5% CO2 and time-lapse imaging with personalized gonadotropin protocols (IU). We monitor follicular development in real time and adjust each step under strict quality controls. Can I continue my treatment between Mexico and the U.S.? Yes. Our integrated network maintains consistency in volumes (mL), temperatures (°C), and your medical history. We coordinate all logistics so you can focus on your health and well-being. What emotional support does Ingenes offer? We have certified psychologists and support groups to manage stress—such as cortisol in µg/dL—that can affect your treatment. At Ingenes, you’re never alone: we provide a warm, supportive environment. Sources Consulted American College of Obstetricians and Gynecologists. (2023). Clinical Management Guidelines. https://www.acog.org MedlinePlus. (2022). In Vitro Fertilization. https://medlineplus.gov/ivf.html Practice Committee of the American Society for Reproductive Medicine. (2021). Definitions of ART Success Rates. Fertility and Sterility, 115(5), 1234-1241. World Health Organization. (2020). WHO Laboratory Manual for the Examination and Processing of Human Semen (6th ed.).

Fertilization with the ICSI method (intracytoplasmic sperm injection) offers higher success rates when one of the factors to address is teratozoospermia: we select a sperm with normal morphology and inject it directly into the egg, optimizing the chances of fertilization. What is teratozoospermia and why is its diagnosis important? Teratozoospermia is a medical term describing a high percentage of abnormally shaped sperm in semen. Teratozoospermia is defined when more than 96% of sperm have altered forms, reducing their motility and ability to penetrate the egg. What causes can lead to teratozoospermia? Semen quality can be affected by various factors: Diabetes mellitus Varicocele Vasectomy over 5 years ago Infections of the seminal tract Testicular problems or trauma Poor nutrition Smoking, alcohol, or drugs Exposure to insecticides and other toxins Advanced age (from 45 years, abnormal sperm increase) Cancer treatments (chemotherapy, radiotherapy) Recent fevers Excess heat (saunas, jacuzzis, vehicle seats) How is teratozoospermia diagnosed and classified? Diagnosis is made with a semen analysis after 3–7 days of abstinence: WHO: at least 4% normal sperm. Kruger: 4–15% normal = moderate teratozoospermia. Less than 4% normal = severe teratozoospermia. Normal sperm have an oval head of 5–6 µm × 2.5–3.5 µm and a flagellum of ~50 µm. What treatments exist to improve fertility? Artificial insemination: capacitated semen in the uterus. For moderate teratozoospermia and women under 35 years. In vitro fertilization (IVF): egg and sperm union in the lab. Recommended if the woman is over 35 years. ICSI: injection of a normal sperm into the egg. The option with the best rates in severe teratozoospermia. A healthy lifestyle enhances semen quality: balanced diet, essential amino acids (L-Carnitine), and antioxidants. Avoid self-medication. For more information on erectile dysfunction and fertility or male infertility and how to conceive a baby, visit our specialized articles. FAQ on teratozoospermia and fertility 1. Can teratozoospermia be corrected with lifestyle changes? In mild or moderate cases, improving habits (balanced diet, exercise, and reducing toxins) can increase the percentage of normal sperm. Antioxidants and L-Carnitine also help. If symptoms persist, consult a specialist. 2. Is ICSI safe for severe teratozoospermia? ICSI manually selects a sperm with good morphology and injects it into the egg, achieving high fertilization and pregnancy rates. Before the procedure, the doctor will assess your history and semen quality. 3. When can improvement be seen after treatment? The sperm production cycle lasts ~72 days, so changes in habits or treatments usually reflect in 2–3 months. Follow-up semen analyses help adjust the plan. 4. Does the man’s age influence the results? Men over 45 years have more abnormal sperm and lower motility. When planning IVF or ICSI, male age is considered to optimize the protocol. Sources consulted World Health Organization. (2021). WHO Laboratory Manual for the Examination and Processing of Human Semen (6th ed.). Cooper et al. (2010). WHO reference values for human semen characteristics. Human Reproduction Update, 16(3), 231–245. Carlsen et al. (1992). Evidence for decreasing quality of semen during past 50 years. BMJ, 305(6854), 609–613. MedlinePlus. (2022). Teratozoospermia. We know this journey can be challenging. Stay hopeful and remember each case is unique. Consulting an assisted reproduction specialist will give you the personalized guidance you need to increase your chances of success.

What is egg freezing and what is it for? Egg freezing is an assisted reproduction technique that helps you pause your biological clock. Your mature oocytes are retrieved and vitrified in liquid nitrogen at –196 °C, where they can be stored for up to 27 years. Avoid self-medicating without consulting a doctor, as each ovarian stimulation protocol is adjusted to your age, ovarian reserve, and health status. How to know if egg freezing is right for you? If you want to postpone motherhood without losing options, this technique is your ally. The first step is to see a specialist in Assisted Reproduction. With an anti-Müllerian hormone (AMH) test and an antral follicle count (AFC) via ultrasound, you’ll assess your ovarian reserve and confirm if it’s the ideal time. What medical reasons drive egg freezing? Besides personal reasons, there are medical situations that make this decision advisable: Chemotherapy or radiotherapy that damages ovarian reserve. Gender transition. Autoimmune diseases or gynecological oncology surgeries. In these cases, vitrifying your oocytes opens a door of hope for your family plans. Do you need a partner to freeze your eggs? No. Unlike embryos, only your oocytes are stored here. If in the future you decide to fertilize them and don’t have a partner, you can use certified donor sperm from a sperm bank. Egg freezing process step by step Ovarian stimulation with hormones (FSH and LH) in personalized doses (e.g., 150–300 IU/day). Ultrasound monitoring and estradiol (E2) measurement in pg/mL. Retrieval of mature oocytes via follicular puncture under sedation. Vitrification of each oocyte with cryoprotectant to prevent ice crystals. Storage in liquid nitrogen tanks (<–196 °C). With Ingenes, your oocytes are protected by a unique chain-of-custody system. Alternatives and next steps In addition to egg freezing, you can consider: Embryo vitrification. Ovarian tissue preservation. We recommend reading “Egg freezing: a strategic decision for your family’s future” to learn how these options fit your life plan. At Ingenes we provide guidance at every stage: freezing eggs means gaining time with warmth and security. Frequently Asked Questions (FAQ) 1. Does egg freezing guarantee a future pregnancy? Success rates vary based on your age at vitrification and oocyte quality. Women under 35 have over 90 % survival after thawing and 50–60 % pregnancy rates per cycle. However, factors like embryo implantation and endometrial receptivity also play a role. That’s why it’s essential to see an Assisted Reproduction specialist. 2. What risks does ovarian stimulation carry? The main risk is ovarian hyperstimulation syndrome (OHSS), with abdominal pain, bloating and, in severe cases, pleural effusion or ascites (< 2 % with modern protocols). Other effects include breast tenderness, mood changes, and mild discomfort during retrieval. At Ingenes we monitor you closely to ensure your well-being. 3. How long can eggs be stored? Vitrification keeps them viable for decades. There are cases of pregnancies after 27 years of storage. Legally, the limit depends on the country: in Mexico it’s up to 10 years, renewable with your consent. 4. Can I change my motherhood plans? Yes. You can use your oocytes with partner or donor sperm in IVF cycles whenever you choose. Also, if the law allows, you can transfer embryos to a gestational carrier. At Ingenes we support you with legal and psychological counseling every step of the way. Sources Consulted Practice Committee of the American Society for Reproductive Medicine. (2020). Mature oocyte cryopreservation: a guideline. Fertility and Sterility, 114(4), 767–781. https://doi.org/10.1016/j.fertnstert.2020.06.025 American College of Obstetricians and Gynecologists. (2018). Committee Opinion No. 745: Patient education and informed consent. Obstetrics & Gynecology, 131, e196–e205. https://doi.org/10.1097/AOG.0000000000002586 MedlinePlus. (2023). Egg freezing. Retrieved from https://medlineplus.gov/eggsfreezing.html European Society of Human Reproduction and Embryology. (2022). ESHRE Guideline: Oocyte preservation. Human Reproduction Open, 2022(1), hoac004. https://doi.org/10.1093/hropen/hoac004 We accompany you on your journey to motherhood and fatherhood. Don’t hesitate to seek the support of a fertility specialist to answer your questions and design a personalized plan. We’re with you!

In this article, we clarify how motherhood and pregnancy are experienced with a disability, and we offer advice for future moms and dads to explore the options provided by Assisted Reproductive Technologies. According to the World Health Organization, disability arises from the interaction between a person’s health conditions and personal or environmental factors. When thinking about disability, one often imagines a wheelchair, but there are actually multiple forms of disability: Physical: difficulties moving. Psychological: cognitive barriers affecting personal or social development. Communication: obstacles to speaking, seeing, hearing, or reading. What does becoming pregnant with a disability entail? 15% of the world’s population lives with some form of disability. In the U.S., 26% of adults have a disability, and 1 in 4 women is affected. Anyone can experience a disability, temporary or permanent. (WHO, 2021) Why is there discrimination against pregnant women with disabilities? Despite progress in equality, a lack of awareness about the daily lives of people with disabilities leads to stigma and discrimination. Everyone has the right to access quality healthcare without distinction. The UN Convention Article 25 guarantees the right to receive excellent medical care without discrimination. How often do women with disabilities become pregnant? Many women with disabilities conceive naturally since their reproductive health functions normally. Only certain conditions, like spinal cord injuries, require Assisted Reproduction. Assisted reproduction options for women with disabilities In cases of quadriplegia or paraplegia, natural conception is usually impossible. The most effective solutions are adapted technologies, such as: Artificial insemination: recommended for those under 35 with normal ovarian reserve and a partner with healthy semen parameters. In vitro fertilization (IVF): higher success rates, ideal for those over 35 or with reproductive challenges. How to prepare for a pregnancy with a disability Planning is crucial. Consult a fertility specialist before a general gynecologist if you’re considering assisted reproduction. Find inspiration in real stories like “Pregnant Together: Overcoming Infertility with Assisted Reproduction” and learn about your rights in reproductive rights and ARTs. Recommendations during pregnancy with a disability Plan with your doctor: set goals and avoid self-medication. Seek testimonials: read experiences like “The Disabled Woman’s Guide to Pregnancy and Birth” or stories on our testimonials blog. Adopt new routines: adapted exercise, balanced diet, or psychological therapy, always under medical supervision. Key questions for your assisted reproduction specialist Before starting any treatment, ask about success rates, risks, medication dosages, and lifestyle changes. Consulting an Assisted Reproduction expert increases your chances of success. References World Health Organization. (2021). Disability and health. Centers for Disease Control and Prevention. (2022). Disability Impacts All of Us Infographic. United Nations. (2006). Convention on the Rights of Persons with Disabilities, Article 25. Rogers, J. (2015). The Disabled Woman’s Guide to Pregnancy and Birth. Frequently Asked Questions 1. Can I Get Pregnant with a Severe Physical Disability? In most cases, fertility is unaffected, except for spinal cord injuries that complicate natural conception. Artificial insemination and IVF are valid options. 2. What Precautions Should I Take for a Safe Pregnancy? Plan with your doctor, maintain a balanced diet, do adapted exercises, and avoid self-medication. Seek support networks and testimonials to feel accompanied. 3. How Do My Reproductive Rights Affect Access to Treatments? Reproductive rights guarantee nondiscriminatory care. UN Convention Article 25 supports your access to comprehensive reproductive health services. 4. Which Technique Has the Highest Success Rate? IVF typically offers better results, especially for those over 35 or with risk factors. Artificial insemination is less invasive and suitable for younger cases with good ovarian reserve. Remember: every case is unique. Always seek guidance from an Assisted Reproduction specialist to receive the best support and increase your chances of success.

Sexual and reproductive education matters to everyone. From adolescence to adulthood, understanding our bodies and health is key. Without proper information, myths arise that can affect our lives. At Ingenes, we believe knowledge gives you the power to live healthier and with hope. What is sexual and reproductive education and why is it important? It’s clear, evidence-based information on anatomy, the menstrual cycle, consent, contraceptive methods (pills with 0.03 mg ethinylestradiol), and STI prevention. We talk about respect and informed decisions to reduce unintended pregnancies and diseases. How does sexual education reduce health risks? It teaches safe practices, like using a condom correctly (0.05 mm latex) and when to see a doctor. Informed people have 50% fewer unintended pregnancies and lower rates of chlamydia and gonorrhea. Do not self-medicate: always seek reliable sources. What does Ingenes do in reproductive health? We focus on fertility within a holistic approach. We offer workshops, webinars, and counseling on menstrual health, hormonal balance (estrogen levels in pg/mL), and fertility. Learn more at World Sexual Health Day. How do we debunk myths and taboos? We dispel ideas like “you can’t get pregnant during your period” or “IVF fails after 40” using studies and expert consensus. We create a shame-free space for you to ask questions and clear doubts. Why does understanding your fertility matter? It’s not just for those who want to conceive. Signals like a 0.3 °C rise in basal temperature or cervical mucus help you plan or address conditions like PCOS. Before taking any medication, consult a reproductive specialist. Tools to improve your reproductive health Use tracking apps (28 ± 2 day cycles), symptom diaries, and regular check-ups. Read also Let’s talk about reproductive health for habits that boost your fertility. Where are we headed? We incorporate findings on endocrine disruptors (ng/kg body weight) and update resources with your voice. We aim for a community of trust and empathy. Knowledge is power. At Ingenes, we accompany you every step of the way. Frequently Asked Questions 1. At what age should it start? From ages 9–10 with information about the body and respect. Over time, topics like consent and contraception are addressed. This lays a solid foundation for decisions in adolescence and adulthood. 2. Does it impact mental health? Yes. Comprehensive programs work on self-esteem, boundaries, and emotions. Well-informed adolescents show less anxiety and depression related to sexuality. 3. What to do with irregular cycles? Record duration, flow, and symptoms. Cycles under 21 days or over 35 may indicate PCOS or thyroid issues. Consult a specialist: they will analyze progesterone (ng/mL) and perform ultrasounds for a personalized plan. 4. Are fertility apps reliable? They help recognize patterns but do not guarantee contraception. Combine them with physical signs and medical guidance for better results. Sources Consulted CDC. Sexual and Reproductive Health. 2022. https://www.cdc.gov/reproductivehealth/index.html MedlinePlus. Menstrual Cycle. 2023. https://medlineplus.gov/menstrualcycle.html WHO. Sexual and reproductive health and research. 2021. https://www.who.int/teams/sexual-and-reproductive-health-and-research ACOG. FAQ: Menstrual Cycle. 2020. https://doi.org/10.1097/AOG.0000000000004066 We are with you on this journey. If you are trying to conceive or have questions, consult a fertility specialist for the best guidance and support.

Progesterone, the hormone driving your dream of becoming a mother or father, is key to female fertility. When it’s lacking, it can become a silent obstacle. At Ingenes we understand how much reaching motherhood or fatherhood means to you, which is why we care for every detail of your hormonal balance. What does progesterone do? Known as “the pregnancy hormone,” progesterone prepares the uterus to receive the embryo and sustains it during the first weeks. Adequate levels create a welcoming environment for implantation and early development. If you think your body needs help, in this article we explain how to detect and correct a possible deficiency. Warning signs Low progesterone shows up as irregular cycles, spotting before your period, or difficulties conceiving. At Ingenes we use precise blood tests (measuring ng/mL) to detect imbalances and give you a clear picture of your reproductive health. Impact on your dertility Without enough progesterone, implantation can fail or the risk of early miscarriage increases. Our team evaluates your hormonal profile and, if necessary, includes studies on the embryo factor to maximize your chances of success. Treatments at Ingenes We offer personalized plans: oral or vaginal progesterone supplements (measured in mg) and, if needed, intrauterine insemination or IVF. Remember: “Do not self-medicate without specialist guidance.” Our approach aims to restore your hormonal balance and create the best conditions to conceive and carry a healthy pregnancy. “Before starting any treatment, consult a Specialist in Assisted Reproduction to increase your chances of success.” If you feel that progesterone is standing in the way of your journey to motherhood or fatherhood, we are here for you. We support you with warmth and expertise every step of the way. Frequently Asked Questions Can low progesterone cause implantation failures? Yes. This hormone prepares the endometrium to nourish the embryo. If levels are low during the luteal phase, the endometrium may be too thin. Measuring progesterone 7 days after ovulation helps determine if supplementation is needed. Sometimes combining progesterone with luteal support in IVF improves implantation rates. Always follow your specialist’s prescribed doses. When should progesterone be measured after ovulation? About 7 days after ovulation (day 21 in a 28-day cycle). It should exceed 10 ng/mL. Blood testing is the most reliable method. If your levels are low, your doctor may recommend 100–400 mg/day of vaginal or oral progesterone. Do not self-medicate; always seek specialist guidance. Natural ways to boost progesterone? An balanced lifestyle helps: a diet rich in vitamin B6 and magnesium, stress control with yoga or mindfulness, and maintaining a BMI between 18.5–24.9. Avoid excessive exercise. But if the imbalance is significant, medical therapy is the safest way to reach optimal levels. Can supplements prevent miscarriage? In women with a weak luteal phase or recurrent losses, vaginal progesterone (200–600 mg/day) may improve the chance of maintaining pregnancy until week 10–12. Speak with your specialist to determine the route, dosage, and duration based on your history. Sources Consulted MedlinePlus. (2023). Progesterone. Retrieved from https://medlineplus.gov/ency/article/003476.htm Nagaraju, S., & Imudia, A. N. (2021). Luteal phase support in assisted reproductive technology. Best Practice & Research Clinical Obstetrics & Gynaecology, 73, 95-103. American Society for Reproductive Medicine. (2022). Progesterone supplementation: Practice Committee opinion. Fertility and Sterility, 118(3), 495-500. MedlinePlus. (2022). Luteal phase defect. Retrieved from https://medlineplus.gov/genetics/condition/luteal-phase-defect We understand you, support you, and trust in your strength. If you need personalized guidance, consult a specialist in fertilization. Your dream of starting a family matters, and you’re not alone on this journey!

Progesterone is an essential hormone on your journey to parenthood, responsible for regulating the menstrual cycle and supporting pregnancy. It is produced mainly by your ovaries after ovulation and, in smaller amounts, by the adrenal glands. Its role is to prepare the uterine lining for embryo implantation and maintain a stable environment during gestation. Do not self-medicate: always consult a professional. What is progesterone and what is it for? Progesterone plays a key role in your body: Regulates your menstrual cycle. Prepares the endometrium for implantation of the fertilized egg. Maintains the uterine lining during pregnancy. Prevents premature contractions. If you are looking to improve your chances of pregnancy, speak with a specialist in Assisted Reproduction. Learn more about this fertility treatment. Progesterone production in the body In women, progesterone is synthesized in: Ovaries: the corpus luteum produces it after ovulation. Placenta: during pregnancy, up to 200 mg/day in the third trimester. Adrenal glands: in both sexes, less than 1 mg/day. Common side effects When taking progesterone supplements, you may experience: Mood swings or feelings of sadness. Breast pain or tenderness. Fatigue and drowsiness. Headaches or migraines. Nausea and digestive discomfort. Fluid retention and weight fluctuations. Irregular bleeding or spotting. Very low risk of thrombosis. Why do these effects occur? Nervous system: alters neurotransmitters, causing emotional changes. Digestive system: slows gastric emptying and intestinal transit. Fluid retention: excess sodium and water cause swelling. The administration route (oral, 100 mg vaginal suppositories, 25 mg/mL injectable) and your individual sensitivity influence symptom intensity. Managing side effects If you notice discomfort, consult your specialist to adjust the dose or change the progesterone form: Keep a symptom diary: frequency and intensity will help your doctor personalize the treatment. Maintain healthy habits: a balanced diet, exercise, and rest improve overall well-being. Practice relaxation techniques: yoga, meditation, or mindful breathing to reduce anxiety. Seek emotional support: talking with family, friends, or groups will make you feel understood. Discover more specialized recommendations. Perspectives in assisted reproduction In fertility, progesterone optimizes uterine receptivity and increases implantation rates. Protocols vary: from 200 mg/day vaginally to 50 mg intramuscularly every 24 h. With the support of assisted reproduction professionals, the dose is adjusted to balance efficacy and comfort. Frequently Asked Questions 1. Does progesterone cause weight gain? Fluid retention can cause moderate, temporary weight gain. Maintain a balanced diet and regular exercise. If significant, consult your doctor to adjust the regimen. 2. Is it safe to use progesterone during the first trimester? It is often prescribed until weeks 12–14 with doses of 200–400 mg/day vaginally to prevent miscarriage. Each case is unique: your specialist will define duration and dose. 3. What alternatives exist if I cannot tolerate the oral route? You can use 100–200 mg vaginal suppositories every 12–24 h or 25–50 mg/mL intramuscular injections, which reduce systemic effects and act directly on the uterus. 4. Can I become pregnant if I have strong side effects? Side effects do not prevent pregnancy. With adjustments and medical follow-up, you can continue treatment without affecting implantation or embryonic development. Sources consulted MedlinePlus. Progesterone. https://medlineplus.gov/druginfo/meds/a604017.html ACOG Practice Bulletin No. 193: Use of Progesterone for Prevention of Preterm Birth. Obstetr Gynecol, 2018. Fertility and Sterility. 2020;114(2):259-270. doi.org/10.1016/j.fertnstert.2020.12.020 WHO. Progesterone for the prevention of preeclampsia. 2019. We understand and support you in this process. For personalized and safe guidance, always consult a fertilization specialist. Best of luck on your path to parenthood!

International Folic Acid Awareness Week is more than an annual event; it’s a global movement aimed at teaching and raising awareness about the importance of this vitamin in reproductive health. Folic acid, the synthetic form of folate, is an essential B vitamin for preventing birth defects and supporting optimal fetal development. It’s key for women planning a pregnancy or already expecting. What is folic acid and why is it crucial before pregnancy? Folic acid, known as vitamin B9, is fundamental for vital functions like DNA replication, cell division, and red blood cell formation. Its role is decisive in the first weeks of gestation, even before you know you’re pregnant, because it helps form the neural tube, the precursor to the baby’s brain and spinal cord. Folic acid deficiency in these early stages can cause neural tube defects such as spina bifida or anencephaly. Do not self-medicate: before starting supplementation, consult a specialist in assisted reproduction, especially if you aim to increase your chances of conceiving. How much folic acid is recommended for fertility? Health experts indicate that women of childbearing age should consume at least 400 µg (micrograms) of folic acid per day. During pregnancy, the dose increases to 600 µg/day. Although folate is present in leafy greens, citrus fruits, and legumes, reaching these amounts through diet alone can be challenging. That’s why folic acid supplements are a practical and effective strategy. Additionally, including folate-rich foods enhances its benefits. Learn more in our article Nutrition Day: How Diet Impacts Your Fertility and Reproductive Health. How does folic acid affect male fertility? Folic acid also benefits men. Studies show that adequate intake improves sperm quality by supporting cell division and reducing chromosomal abnormalities. This way, it increases the probability of conception. Best practices for supplementing with folic acid Start at least 3 months before trying to conceive. Maintain a consistent intake throughout the entire pregnancy. Combine supplementation with a balanced, folate-rich diet. Always consult a specialist before self-medicating. Why is nutrition vital in fertility treatments? Diet directly influences reproductive health. Learn how nutrients and lifestyle can enhance your fertility treatment outcomes in our article The Importance of Nutrition in Fertility Treatment. At Ingenes, we offer a personalized, evidence-based guide to support you on the path to a healthy pregnancy. Frequently Asked Questions Can I Take More Than 600 µg of Folic Acid Safely? Exceeding 600 µg/day provides no additional benefits and can mask symptoms of vitamin B12 deficiency. Consult your doctor to establish the optimal dose based on your health status and medical history. Each woman has individual needs, especially if she has anemia or a history of neural tube defects. What Is the Difference Between Folate and Folic Acid? Folate is the natural form found in spinach, broccoli, and legumes, while folic acid is the synthetic version in supplements and fortified foods. Both perform similar functions, but folic acid has higher bioavailability when taken on an empty stomach. A folate-rich diet provides additional nutrients, so combining both sources is the most effective strategy to meet daily recommendations. When Should I Stop Taking Folic Acid? It’s recommended to continue supplementation until the end of the first trimester, when the neural tube is fully formed. After that, your doctor will assess whether to maintain a lower dose or switch to a multivitamin. Do not stop folic acid on your own: your specialist will determine the ideal supplementation plan based on your pregnancy’s progress. Does Folic Acid Prevent All Birth Defects? Folic acid significantly reduces the risk of neural tube defects but does not prevent all congenital anomalies. Other genetic, environmental, and nutritional factors also play a role. Along with supplementation, maintain a healthy lifestyle, avoid toxins, and attend prenatal checkups to detect and manage potential risks early. Sources Centers for Disease Control and Prevention. (2023). About Folic Acid. Retrieved from https://www.cdc.gov/ncbddd/folicacid/about.html World Health Organization. (2018). WHO recommendations on antenatal care for a positive pregnancy experience. Geneva: WHO. doi:10.1016/S0140-6736(19)30212-1 U.S. National Library of Medicine. (2022). Folic Acid. MedlinePlus. Retrieved from https://medlineplus.gov/folicacid.html Blum, J. W., & Garza, C. (2016). Folate supplementation and prevention of neural tube defects. The Lancet, 388(10057), 1427–1429. doi:10.1016/S0140-6736(16)21555-4 We know the journey to motherhood and fatherhood can be exciting and challenging. You are not alone! If you have questions or need a personalized plan, consult a fertilization specialist to receive the right guidance and give your future baby the best start.

In a society where turning 40 without a partner but with the dream of becoming a mother may seem challenging, we want to remind you that this stage is not the end, but the beginning of a journey full of hope. Here you will find clear and approachable information about your fertility options and how Ingenes accompanies you step by step. How does being 40 affect my fertility and what can I do? At 40, ovarian reserve decreases by about 3% each year after 35, but that doesn’t close the door on motherhood. At Ingenes we analyze your hormonal profile, anti-Müllerian hormone levels (AMH in ng/mL) and antral follicle count (AFC) to offer you a fully personalized plan. In vitro fertilization (IVF) is one of the most effective alternatives. In this process, sperm and eggs are combined in 2 mL of culture medium per egg and cultured to the blastocyst stage. With implantation rates that can exceed 40% in women under 42, stories like this experience show how encouraging the journey can be. What is egg donation and when is it recommended? Egg donation involves using eggs from a young, healthy donor for IVF. It’s ideal if your AMH is below 1 ng/mL or if you’ve had failed implantation attempts. At Ingenes we support you from donor selection, genetic testing (PGT-A) and cycle synchronization, to embryo transfer. Cases like this single mother at 43 speak of positive results and renewed confidence. How can I prepare for motherhood after 40? Becoming a mom at 40 requires emotional and practical preparation. Adjust your home to welcome the baby and organize your routine with 8 hours of sleep and moments for yourself. Consult a nutritionist: a diet of 1,800–2,200 kcal daily, with 1.2 g/kg of protein, 400 µg of folic acid and 18 mg of iron. A reproductive endocrinologist will adjust doses and supplements and remind you not to self-medicate. Why is emotional support essential? Waiting, hormones and results can generate anxiety. At Ingenes we have psychologists who use cognitive-behavioral therapy so you can manage stress and strengthen your resilience. A MedlinePlus study (2022) shows that emotional support improves treatment adherence by 30%. Remember: before taking any medication, consult a reproductive specialist. What are the risks and benefits of being a mother after 40? Risks include preeclampsia or gestational diabetes (up to 20%) and a slight increase in chromosomal abnormalities. That’s why we recommend non-invasive prenatal testing (NIPT) and, if necessary, amniocentesis. Benefits include economic and emotional stability, greater maturity and a consolidated support network, which make parenting easier. How do I care for my mental health during the process? Mental health is as key as physical health. Practice mindfulness or prenatal yoga to lower cortisol by up to 25%. Join support groups: sharing removes loneliness. If you experience emotional swings, seek professional help. At Ingenes we collaborate with perinatal psychiatrists who provide the necessary support under supervision. What physical health habits promote a healthy pregnancy? Do moderate exercise (30 minutes daily of walking or swimming) and periodic check-ups with your gynecologist. Monitor your blood pressure and glucose every trimester. Avoid tobacco and alcohol, limit caffeine to 200 mg/day and maintain a BMI between 18.5 and 24.9 kg/m² to optimize implantation. How to financially plan motherhood as a single mother at 40? The cost of IVF with egg donation ranges from USD 8,000 to 12,000. Add consultations, hormones (~USD 1,200 per cycle) and genetic tests. Create a monthly budget that includes childcare, insurance and emergency savings. A financial advisor can help you plan long term. Choosing to become a mother at 40 is an act of courage. At Ingenes we support you with cutting-edge technology and comprehensive care: emotional, physical and financial. We’re here to turn your dream into reality. Frequently Asked Questions What is the success rate of IVF in 40-year-old women? The average success rate of IVF in 40-year-old women ranges from 25% to 35% per cycle. With advanced techniques like PGT-A, Ingenes has reached up to 40% in optimal cases. Every case is unique; your personalized protocol can improve these results. How long does the entire assisted reproduction process take? From initial analysis to embryo transfer takes 4 to 6 weeks: hormone studies, ultrasounds every 3–4 days, ovarian stimulation with FSH/LH and follicular puncture under local anesthesia. With egg donation it can extend to 8 weeks due to cycle synchronization. Is the follicular puncture procedure painful? It is performed under local anesthesia or light sedation, and most experience minimal discomfort. After the procedure you may have cramps or swelling that resolve in 24–48 hours. We prescribe paracetamol 500 mg every 6 hours and recommend relative rest for 48 hours. Our team is available 24/7. Can I donate my own eggs if successful and share them with other women? At Ingenes we follow anonymity and consent guidelines. A patient may not donate her eggs after a personal cycle. However, you can participate in “solidarity donation” programs after a 3-month recovery period and medical and psychological criteria are met. Sources American Society for Reproductive Medicine. (2023). Fertility Facts and Figures. https://www.asrm.org/ MedlinePlus. (2022). Assisted Reproductive Technology. https://medlineplus.gov/assistedreproductivetechnology.html Practice Committee of the American Society for Reproductive Medicine. (2021). Role of Donor Egg IVF. Fertility and Sterility, 115(2), 301–307. https://doi.org/10.1016/j.fertnstert.2020.12.031 World Health Organization. (2020). WHO recommendations on infertility interventions. https://www.who.int/publications/i/item/9789241550173 We accompany you at every step of this journey. If you have questions or want to start your treatment, consult an assisted reproduction specialist. We’re here to help you fulfill your dream of becoming a mother or father!

Today, infertility rates have risen in the Mexican population. It is estimated that 20% of people face sterility issues, a challenge that deserves specialized attention to improve the quality of life for many families. Why is research in assisted reproduction key to combating infertility? Research and development laboratories are the heart of advances in reproductive medicine. There, data are collected and analyzed to refine protocols, techniques, and outcomes. Findings not only confirm current knowledge but also generate new information that drives the entire field. At the Ingenes Institute, we have state-of-the-art laboratories dedicated to developing techniques that increase pregnancy chances and bring many families closer to the dream of having a baby. How do next-generation laboratories improve fertility outcomes? At Ingenes, we integrate technological innovation at every stage of your care. By combining empirical observation with international methodologies, our team adjusts protocols to: Increase pregnancy success rates. Optimize embryo selection and transfer. Personalize treatments with molecular diagnostics. Each case is unique, which is why we provide exclusive care and design strategies that maximize your chances of conception. What is preimplantation genetic diagnosis and how does it work? Preimplantation Genetic Diagnosis (PGD) is performed on embryos created via IVF. Using comparative genomic hybridization (CGH) technology, it detects genetic or chromosomal abnormalities before transfer, increasing the likelihood of a healthy pregnancy. A cell from the embryo is biopsied, its DNA amplified, and analyzed on microarrays to identify anomalies. This technique, used worldwide, has significantly improved pregnancy rates. Before starting any medication or procedure, consult a reproductive specialist. How is endometrial receptivity tested and why does it matter? The endometrial receptivity test analyzes RNA from the uterine lining using qRT-PCR. This minimally invasive molecular evaluation determines the optimal window for embryo implantation. Knowing the exact moment the endometrium is most receptive helps schedule the transfer and maximize success chances. What new methods exist to assess egg quality? Oocyte quality is key to female fertility. Traditional morphological evaluation can be subjective. Our researchers develop novel molecular markers to accurately measure each egg’s integrity. These techniques aim to identify viability biomarkers and enable personalized interventions. Where can I find more answers about an accurate fertility diagnosis? Discover the Keys to an Accurate Diagnosis in the Search for Fertility and learn how advanced studies can guide your path to the right treatment. For frequently asked questions, visit our Most Searched Fertility Questions on Google, where we address concerns and dispel myths. What research projects are shaping the future of assisted reproduction? At Ingenes, we are working on comparative genomic analysis of fetal cells and sex diagnosis to prevent sex-linked diseases. These studies will expand our knowledge of early development and inheritance patterns, contributing to safer and more effective fertility treatments. Maintaining a comprehensive approach that combines multiple techniques is our goal to accompany you on the path to parenthood. Avoid self-medication and always consult a physician. What support will I receive during my fertility journey? We offer psychological support, nutritional counseling, and guidance at every stage. Our team provides clear explanations and emotional care, because we understand the challenges of infertility and share your desire to become a mother or father. FAQ 1. What diagnostic tests should I consider before IVF? Before IVF, it is essential to assess ovarian reserve with hormones (AMH, FSH) and antral follicle count via transvaginal ultrasound. A hysterosalpingography (HSG) should also be performed to check fallopian tube patency and detect uterine anomalies. These studies offer a comprehensive view of your reproductive health. Genetic tests, such as karyotyping for both partners, can reveal chromosomal translocations affecting the embryo. Reviewing medical history, surgeries, or previous infections also helps design a personalized IVF protocol. 2. How long does preimplantation genetic diagnosis take? The PGD process takes 7 to 10 days. Embryos are cultured to day 5 or 6 (blastocyst stage), a cell is biopsied, and sent to the genetic laboratory. DNA amplification and microarray analysis take 48 to 72 hours. With the results, healthy embryos are selected for transfer. Quick turnaround minimizes the embryo’s time outside the uterus, maintaining viability. Your specialist coordinates everything so the plan aligns with result delivery. 3. Can the endometrial receptivity test fail? Although qRT-PCR–based tests have over 95% accuracy in determining the implantation window, no test guarantees pregnancy. Factors such as embryo quality, uterine anatomy, or immunological conditions also play a role. However, endometrial receptivity testing significantly reduces the risk of out-of-phase transfers. Combining these results with embryo genetic screening further improves success rates. 4. Are there noninvasive ways to assess embryo health? Metabolomic profiling in culture media is being investigated by analyzing molecules released by the embryo (amino acids, lipids). This approach could predict implantation potential without biopsies. Initial studies show promising correlations between metabolic signatures and embryo viability. Integrating time-lapse imaging and artificial intelligence also enables noninvasive evaluation by tracking developmental milestones and morphological changes in real time. References American Society for Reproductive Medicine. Practice Committee. (2022). Guidance on the use of preimplantation genetic testing. https://doi.org/10.1016/j.fertnstert.2022.01.004 MedlinePlus. (2023). Endometrial receptivity assay. https://medlineplus.gov/ency/article/003610.htm ACOG. (2021). Assessment of ovarian reserve. Obstetrics & Gynecology, 137(2), e117–e129. https://doi.org/10.1097/AOG.0000000000004256 ESHRE. (2020). Embryo selection: time-lapse and non-invasive testing. Human Reproduction Open, 2020(hoaa024). https://doi.org/10.1093/hropen/hoaa024 We are with you every step of the way. Remember: seeking professional help is essential to make safe and successful decisions in your parenthood journey.

At Ingenes we know very well the concerns of couples seeking their first child. We understand the stress and frustration when suspecting there may be some degree of infertility. Today we address especially couples who have been trying for more than 12 months without success, with particular attention to the male factor. Male infertility is rarely acknowledged. Thinking about it generates discomfort, anger, disbelief, and sometimes depression; as if you weren’t “man enough.” The truth is these problems are more common than you think and yet remain hidden. Accepting the possibility of a male issue is difficult. If you’ve been trying for 12 months without success, timing and diagnosis are key: an early finding usually leads to better results. Main male causes of infertility Many factors are involved in achieving a pregnancy. If any fail, infertility can occur. In approximately 50% of cases, there is a male component, since half of the embryo’s genetic material comes from the sperm source. Sperm production and function disorders Anejaculation (absence of ejaculation) Asthenozoospermia (low motility) Azoospermia (absence of sperm) Teratozoospermia (abnormal morphology) Varicocele (dilated veins in the scrotum) Seminal infections (e.g., prostatitis) Other conditions affecting fertility Diabetes mellitus (affects nerves and blood flow) Erectile dysfunction (impedes ejaculation) Vasectomy (surgical sterilization) At Ingenes we have cutting-edge technology to address these conditions and offer comprehensive emotional support, essential for treatment success. The first step is to schedule a consultation to diagnose and treat the root cause. Do not self-medicate: always see an assisted reproduction specialist before taking any medication. Influence of emotional health on male infertility Stress, anxiety, and depression alter hormones that regulate sperm production. A supportive environment lowers cortisol and balances testosterone, improving sperm parameters. Learn more about emotional support in assisted reproduction treatments. Creating a support network strengthens couples to face the process together, fostering hope and resilience. Frequently Asked Questions on the Emotional Process in Male Infertility 1. Why acknowledge infertility emotionally? Understanding the emotional impact helps address guilt, shame, or frustration before they become chronic anxiety or depression. This improves treatment adherence and increases reproductive success rates. Also, addressing these feelings with a psychologist or in a support group reinforces couple communication, creating an environment of mutual understanding. 2. What coping strategies help manage stress? Cognitive-behavioral therapy teaches relaxation techniques and the restructuring of negative thoughts. Regular exercise, meditation, and yoga reduce cortisol and boost mood. Participating in support groups or couples therapy allows you to express emotions and share experiences with others in similar situations. 3. How to talk to your partner without causing conflict? Choose a calm moment, express your feelings using “I” statements, and validate their emotions. Avoid accusations and comparisons with other couples. Seeking joint guidance from a specialist provides a neutral space to raise questions and develop a collaborative action plan. 4. When should you seek psychological help? If sadness, anxiety, or irritability persist for more than two weeks, affect your daily life or your relationship, it’s time to consult a mental health professional. A psychologist specializing in reproductive health will evaluate your case and recommend individual or couples therapy to maintain your emotional balance during treatment. Sources American Society for Reproductive Medicine. (2022). Male Infertility: Practice Committee Opinion. Fertility and Sterility. doi:10.1016/j.fertnstert.2022.01.027 Centers for Disease Control and Prevention. (2023). Infertility FAQs. https://www.cdc.gov/reproductivehealth/infertility/index.htm National Institute of Diabetes and Digestive and Kidney Diseases. (2021). Male Infertility. https://www.niddk.nih.gov/health-information/urologic-diseases/male-infertility MedlinePlus. (2024). Infertility. https://medlineplus.gov/infertility.html Remember that your path to parenthood can be consolidated with professional support. You are not alone: consult an assisted fertilization specialist to guide and accompany you every step of the way.
Human Papillomavirus (HPV) can cause significant complications, but did you know it might influence fertility? Although HPV does not directly prevent a woman from conceiving, cervical lesions or cervical cancer caused by the virus could affect her reproductive capacity. In men, there is evidence that HPV may alter sperm quality, although the data remain limited. What is HPV and how does it affect female fertility? In general, HPV does not prevent conception, but if it causes cervical changes or cervical cancer, fertility can be affected. Procedures such as conization or LEEP remove affected tissue and can alter cervical mucus, making it harder for sperm to pass. Chemotherapy or radiotherapy used for cancer can reduce ovarian reserve. HPV detection is done through Pap smears and viral DNA tests. If abnormalities are found, colposcopy and biopsy guide treatment. Do not self-medicate; always consult your doctor. Can HPV affect male fertility? Some studies show that HPV can adhere to sperm, reduce motility, and increase DNA fragmentation. A 2011 article in Fertility and Sterility found lower progressive motility and higher early embryo loss in HPV-positive samples. If you have a persistent infection, consult a fertility specialist before making any treatment or medication decisions. Assisted reproductive technologies and HPV In vitro fertilization (IVF) is an option for couples with HPV. Although some studies report slightly lower implantation and pregnancy rates, techniques such as sperm washing and embryo culture help reduce viral load. Talk to your embryologist to design a personalized protocol. More information at Vaginal Infections and Their Impact on Female Fertility. HPV vaccination and fertility The HPV vaccine prevents high-risk strains associated with lesions and cervical cancer. There is no evidence it harms ovarian function or fertility; by protecting you from the virus, you also safeguard your reproductive health. Vaccination is recommended up to age 26, and in some cases up to 45. Consult your doctor to choose the best timing. Preventive measures and screening tests Use condoms in every sexual encounter and get your screening tests: Pap smear every 3 years or co-testing (Pap smear plus HPV DNA test) every 5 years between ages 30 and 65. Early detection of HPV-related changes allows for less invasive treatments and better fertility outcomes. Don’t forget booster doses if needed. For more pregnancy and HPV tips, visit HPV and Pregnancy: What You Should Know. Frequently Asked Questions Can HPV Be Eliminated on Its Own and Restore Fertility? Yes. The immune system usually clears low-risk strains within 12–24 months without causing permanent cervical damage. If no lesions appear, fertility remains intact. High-risk strains can cause lesions that require treatment. Early follow-up reduces the risk of invasive procedures. Lifestyle Changes That Support Fertility with HPV A diet rich in antioxidants (vitamins C and E, folate), regular exercise, good rest, and stress-reduction techniques (yoga, meditation) strengthen reproductive health. Avoid smoking and limit alcohol, as they promote HPV persistence and affect fertility. How Long After Treatment Can I Try to Conceive? After conservative treatments (LEEP, cryotherapy), wait 3 to 6 months to allow cervical healing and reduce preterm birth risk. If you undergo aggressive treatments or chemotherapy, your specialist will assess your ovarian reserve and may recommend egg or embryo freezing before starting. Is Assisted Reproduction Safe If I Have HPV? Yes. Clinics use sperm or embryo washing and careful culture protocols to minimize viral load. Ask about success rates and additional steps with your specialist. Sources Centers for Disease Control and Prevention. (2023). HPV and Cancer. https://www.cdc.gov/hpv/ Münger, K., & Howley, P. M. (2002). Human papillomavirus immortalization and transformation functions. Virus Research, 89(2), 213–228. MedlinePlus. (2022). Human Papillomavirus (HPV). https://medlineplus.gov/hpv.html World Health Organization. (2021). Human papillomavirus (HPV) and cervical cancer. https://www.who.int/news-room/fact-sheets/detail/human-papillomavirus-(hpv)-and-cervical-cancer We know this journey can raise questions and mixed emotions. You are not alone: every case is unique and solvable. Reach out to an assisted reproduction specialist for personalized guidance and professional support.

Male infertility is present in over 40% of couples experiencing difficulty conceiving. A testicular biopsy helps determine the cause and act precisely so nothing stands in the way of your dream of becoming a father. What is male infertility and how is it detected? Male infertility encompasses any alteration in sperm concentration, motility, or morphology. The first step is a semen analysis that measures: Ejaculate volume (mL) Sperm concentration (million/mL) Sperm motility (%) and morphology (%) If after 12 months of regular, unprotected intercourse pregnancy hasn’t occurred, or if you’ve had recurrent miscarriages, consult an Assisted Reproduction specialist. Avoid self-medication and seek professional guidance. For a complete diagnosis, review our guide on keys to an accurate diagnosis. When is a testicular biopsy indicated? It’s recommended when the semen analysis shows: Azoospermia: total absence of sperm Oligospermia: low concentration (< 15 million/mL) Chromosomal or structural semen abnormalities It’s also useful in cases of vas deferens obstruction (due to vasectomy or malformation), cystic fibrosis, or infections. The biopsy yields testicular tissue to analyze sperm production and, if possible, use sperm in Assisted Reproduction treatments. Fertility expert at the Ingenes Laboratory. How is a testicular biopsy performed? It’s a minor procedure lasting 30–45 minutes: Local anesthesia in the scrotum 2–3 mm incisions in the testicular skin Extraction of tissue fragments (5–10 mg each) Suturing with absorbable or self-dissolving stitches Sending the sample to the Andrology laboratory The embryologist examines the seminiferous tubules under a microscope to locate sperm. If viable sperm are found, they can be used in intracytoplasmic sperm injection (ICSI) during IVF. What will you feel after the biopsy? In the first 48–72 hours it’s normal to experience: Mild to moderate discomfort in the testicular area Scrotal swelling or edema Bruising or small hematomas These symptoms improve within a week with relative rest and mild analgesics. Avoid high-impact sports and sexual activity until your specialist approves. How does the testicular biopsy aid your treatment? If we retrieve sperm, we use them in techniques like ICSI to fertilize eggs in vitro and increase your chances of a successful pregnancy. Always consult an Assisted Reproduction specialist before this step. With an accurate diagnosis, you’ll choose the most successful treatment in the shortest possible time. Frequently Asked Questions (FAQ) 1. Is a testicular biopsy painful? Local anesthesia minimizes pain. Afterwards, mild discomfort may occur, relieved by common analgesics. Most patients recover in less than a week. If you experience intense pain, fever, or excessive bleeding, contact your doctor immediately. Do not self-medicate. 2. When will I have the results? Histological analysis takes 48–72 hours. The pathologist assesses spermatogenesis, atrophy, and possible abnormalities. With the results, your specialist will propose the most suitable treatment plan. 3. Is it safe? It’s a low-risk procedure (complications < 1%). Inflammation, infection, or mild bleeding may occur. To reduce risks, follow pre- and postoperative instructions: hygiene, rest, and supportive underwear. 4. Can I recover natural sperm production? If the issue is reversible (infection, varicocele, or partial obstruction), production may improve after surgical treatment or antibiotics. In non-obstructive azoospermia, direct extraction and IVF are options. Your specialist will guide you based on the diagnosis. Sources Consulted Practice Committee of the American Society for Reproductive Medicine. (2019). Diagnostic evaluation of the infertile male. Fertility and Sterility, 112(4), 687–701. MedlinePlus. (2022). Testicular Biopsy. U.S. National Library of Medicine. Kumar, N., & Singh, A. K. (2015). Trends of male factor infertility. Journal of Human Reproductive Sciences, 8(4), 191–196. World Health Organization. (2021). WHO laboratory manual for the examination and processing of human semen (6th ed.). Remember that every case is unique. We’re with you on this journey and recommend consulting a fertilization specialist for the most appropriate guidance and treatment.

Sexual dysfunctions can be uncomfortable to discuss, but they affect many couples and single individuals. These disorders, in both men and women, impact emotional and physical well-being and relationships. Recognizing and understanding them is the first step to restoring intimate harmony. Sexual dysfunctions: what they are and how they manifest Sexual dysfunction occurs when there are difficulties in any phase of the sexual response cycle (desire, arousal, orgasm, or resolution) that prevent full enjoyment. This can cause stress, frustration, and tension in the relationship. Most common types They can appear at any adult stage: Inhibited sexual desire: Little or no motivation to engage in sexual activity. Erectile dysfunction: Difficulty achieving or maintaining an erection. Premature or delayed ejaculation: Ejaculating in less than 1 minute or taking more than 30 minutes. Dyspareunia and vaginismus: Pain during intercourse, measured on a 0 to 10 scale. Causes and treatments Causes: Physical (diabetes, cardiovascular issues, hormonal imbalances, medications) or psychological (stress, anxiety, depression), or a combination of both. Treatments: Psychological therapy, medications such as PDE5 inhibitors, vacuum devices, or couples therapy. Never self-medicate; always consult an assisted reproduction specialist. The value of professional support Talking with your partner and a specialist is essential. At Ingenes we offer a warm, personalized approach, evaluating your medical, emotional, and relationship history to design the best plan. We have advanced fertility and sexual health technologies, as well as resources on common fertility challenges and support therapies that improve your chances of success. Steps to get started today Consult an assisted reproduction specialist. Undergo emotional and physical assessments with lab tests. Consider couples or individual therapy. Keep a sexual diary to identify patterns. Frequently asked questions 1. When should I seek help? If symptoms persist for more than six months and cause distress, see a doctor. Early diagnosis (with hormonal tests and imaging studies) improves outcomes. Do not minimize symptoms like lack of desire or pain; avoid self-medication and seek an assisted reproduction specialist if you plan to conceive. 2. Are treatments safe when trying to conceive? Some medications may affect fertility. That’s why specialist supervision with evidence-based protocols and precise dosages is key. 3. Why psychological therapy? Cognitive-behavioral and couples therapy reduce anticipatory anxiety and improve communication. Around 60–70% of patients see improvement after 10–15 sessions, especially when addressing trauma or negative beliefs. 4. Are vacuum devices safe? They are effective and non-invasive, with up to 80% satisfaction. They generate negative pressure (mmHg) to improve blood flow. Use under medical supervision to avoid injuries, respecting the maximum time (30 minutes per session). Sources Consulted American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.). doi.org/10.1176/appi.books.9780890425596 NIH. (2023). Sexual Dysfunction. MedlinePlus. https://medlineplus.gov/sexualdysfunction.html Porst, H., & Sharlip, I. D. (2005). Journal of Sexual Medicine, 2(1), 26–35. doi.org/10.1111/j.1743-6109.2005.20102.x Rosen, R. C., et al. (2000). FSFI: Journal of Sex & Marital Therapy, 26(2), 191–208. doi.org/10.1080/009262300278597 Remember: you are not alone. Open communication and professional help bring you closer to intimate well-being and your goal of becoming a parent. See a fertilization specialist for expert, personalized guidance.

Una reserva ovárica baja puede comprometer tus probabilidades de tener un bebé. Te decimos cómo conocer la tuya y tus opciones para ser mamá.

The topic of infertility raises many questions for those trying to have a baby who haven’t succeeded yet. Most turn to the Internet because it’s a free and easy-to-access resource. At Ingenes we researched the most frequently asked questions on Google about infertility and, with the help of our fertility specialist, Dr. Ana Carolina Salazar, we answered each one. What is the difference between sterility and infertility, and why does it matter? “We talk about sterility when a woman under 35 fails to achieve a positive pregnancy test after one year of attempts without contraception and with regular intercourse. If she is over 35, that period is reduced to six months,” explains Dr. Salazar. “Infertility, on the other hand, is the inability to carry a pregnancy to term.” Understanding this difference helps set realistic goals and take the right next step on your reproductive journey. Avoid self-medicating and always consult a specialist. At what age should a woman’s reproductive age be considered, and what factors influence it? “Reproductive age varies from family to family, but on average the best time to try for a pregnancy is before age 32. After that, although possible, the chances decrease,” says Dr. Salazar. Genetic inheritance, ovarian reserve, and lifestyle habits affect that age. Before taking any medication, consult a specialist in Assisted Reproduction to increase your chances of success. How do you know if a woman has the potential to have children? “There are several tests to identify infertility factors. If a tubal issue is suspected, a hysterosalpingography is recommended. If the factor is ovarian, AMH tests and antral follicle count (AFC) are ordered to assess ovarian reserve,” details Dr. Salazar. These tests (AMH in serum mL or follicle count by ultrasound) allow personalizing the treatment plan. At Ingenes we do this through our Initial Program. What are the chances of getting pregnant with Clomiphene and who is a candidate? “Success with Clomiphene depends on the cause of infertility, since it only stimulates ovulation. If you are a candidate, there is a higher risk of multiple pregnancies, so it should always be used under medical supervision,” advises Dr. Salazar. Success rates are around 20–25% per cycle under supervision. Protocols start with 50 mg daily and can go up to 150 mg, always under a specialist’s watch. What is endometriosis, how does it affect fertility, and how is it treated? “Endometriosis is increasingly common in women of reproductive age and one of the main causes of infertility. It involves the growth of endometrial tissue outside the uterus, affecting egg quality and embryo implantation,” explains Dr. Salazar. Management may include laparoscopic surgery, hormonal treatments, or assisted reproduction techniques. Learn more at Research in Search of Answers to Infertility. How to prepare for a comprehensive fertility assessment? According to the National Population Council (CONAPO), 17% of women of reproductive age in Mexico suffer from infertility and at least 1.4 million Mexicans require Assisted Reproduction. Before your first consultation: Keep a menstrual diary for at least three months. Record irregularities in duration or flow (mL of blood). Gather your medical and family history, including BMI (kg/m²). These data help design an individualized evaluation plan. Have you been trying to conceive for more than a year without success? At Ingenes we understand your situation, which is why we created the Initial Program to accurately diagnose and define the shortest path to having your baby. Our Assisted Reproduction specialists have the experience to address each case with the care you deserve. We’re here to help you achieve your dream. If you want a consultation with our experts, tell us your case here and we will be happy to advise you. Frequently Asked Questions 1. Can lifestyle changes improve fertility? Yes. A balanced diet rich in antioxidants, a healthy BMI (18.5–24.9 kg/m²), and avoiding excessive tobacco or alcohol improve outcomes. Moderate exercise (150 minutes per week) helps hormonal balance. Stress-reduction techniques like yoga or mindfulness can boost ovulation. These changes complement but do not replace medical evaluation. Avoid self-medication. 2. When should a couple seek a fertility evaluation? Couples under 35 should evaluate after one year of unprotected intercourse without conceiving. Those over 35 after six months. Early evaluation includes a hormonal panel (FSH, LH, estradiol in IU/L) and anatomical studies such as hysterosalpingography. Timely diagnosis increases treatment success and reduces time to achieve pregnancy. Always consult an Assisted Reproduction specialist. 3. What tests are essential for male fertility evaluation? Semen analysis is fundamental: volume (mL), concentration (million/mL), motility (%), and morphology (% normal forms). DNA fragmentation index and hormone levels (testosterone, FSH, LH) are also assessed. Depending on results, scrotal ultrasound or genetic studies may be required. Evaluating both partners simultaneously avoids unnecessary delays. 4. How do assisted reproduction techniques vary according to diagnosis? Intrauterine insemination (IUI) is for mild male factors or unexplained infertility and involves placing washed sperm (1–2 mL) directly into the uterus. In vitro fertilization (IVF) is used for tubal blockage, severe male factor, or endometriosis, involving egg retrieval and embryo culture. Intracytoplasmic sperm injection (ICSI) is added when sperm parameters are very low. The choice of treatment depends on each case and should be made with a specialist. More information in our Assisted Reproduction FAQs. Sources Consulted Practice Committee of the American Society for Reproductive Medicine. (2020). Definitions of infertility and recurrent pregnancy loss. Fertility and Sterility, 113(4), 533–535. doi:10.1016/j.fertnstert.2019.12.019 National Institute of Child Health and Human Development. (2021). Hysterosalpingography. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMCxxxxxxx/ MedlinePlus. (2022). Clomiphene. Retrieved from https://medlineplus.gov/druginfo/meds/a682097.html World Health Organization. (2010). WHO laboratory manual for the examination and processing of human semen (5th ed.). Geneva: WHO Press. We know how difficult this journey is. Don’t lose hope: every case is unique and there are options within your reach. See a fertilization specialist for the guidance and support you deserve.

The Human Papillomavirus (HPV) is one of the most common sexually transmitted infections worldwide. If you’re pregnant or planning for a baby, it’s natural to wonder how HPV might affect your pregnancy and your little one’s health. Here we clear up those doubts. What is HPV and how does it affect pregnancy? HPV includes more than 200 different viruses. Some cause warts and, in very rare cases, can lead to cancer. Most infections clear on their own within 12 to 24 months without symptoms. Knowing your specific strain helps you and your doctor make the best decisions for your reproductive health. Studies show that HPV itself usually doesn’t complicate pregnancy. Only certain high-risk strains slightly increase the likelihood of preterm birth. The good news is that the vast majority of women with HPV have healthy pregnancies and babies. How does HPV influence pregnancy outcomes? Some research suggests that persistent HPV may be associated with premature rupture of membranes before term (PPROM). But every body is different: your immune system, possible co-infections, and the quality of your prenatal care make a difference. Staying up to date with your appointments helps catch and address any changes early. At Ingenes we focus on personalized care. Avoid self-medication and always consult a reproductive health specialist before starting any treatment. Do not take medications without medical supervision. Can HPV be transmitted to the baby during delivery? Vertical transmission is rare but possible. If it occurs, the newborn could develop laryngeal papillomatosis (warts in the airway) or skin lesions. Early diagnosis and follow-up with a specialist pediatrician allow timely treatment and fewer complications. If your HPV test is positive, discuss delivery options with your obstetrician. In some cases, a cesarean may be considered to reduce exposure, although most vaginal births proceed without issues. How can I protect myself from HPV before and during pregnancy? The HPV vaccine is the most effective tool. It’s recommended before becoming sexually active and covers high-risk strains linked to cervical cancer. If you’re pregnant, vaccination is usually postponed until after delivery. Consult your gynecologist before starting any treatment. Also, using barrier methods (condoms) in every sexual encounter and getting regular tests (Pap smears and HPV DNA) strengthens your defense. For more details on fertility, check our article Human Papillomavirus (HPV) and Fertility. To learn how other infections interact with assisted reproduction, explore Coronavirus and Assisted Reproduction: What You Need to Know. Frequently Asked Questions Can HPV Increase the Risk of Preterm Birth? Some studies indicate that high-risk strains might slightly raise the chance of premature rupture of membranes (PPROM), which can trigger early delivery. However, your overall health, nutrition, and prenatal care are key factors. Keep your appointments on schedule and consult your doctor if you test positive. Is the HPV Vaccine Safe During Pregnancy? Current guidelines recommend postponing vaccination until after delivery, as safety data in pregnancy are limited. If you start the series and then discover you’re pregnant, complete it postpartum. Talk to your gynecologist to plan the best timing. What Should I Do If I Test Positive for HPV While Trying to Conceive? It’s normal to feel concerned. First, don’t self-medicate: see a reproductive health specialist for colposcopy or HPV typing. This will identify any high-risk strains and guide monitoring. Also support your immune health with a balanced diet, moderate exercise, and stress management. How Often Should I Get HPV Tests? It depends on your age and previous results. Between ages 21 and 29, a Pap smear every three years is recommended. From 30 to 65, co-testing (Pap smear plus HPV DNA) every five years offers greater sensitivity. If you have a history of abnormal results or immunosuppression, your doctor may suggest more frequent monitoring. Sources Centers for Disease Control and Prevention. (2023). Human Papillomavirus (HPV) Vaccination: What Everyone Should Know. https://www.cdc.gov/hpv/parents/vaccine.html National Cancer Institute. (2022). Cervical Cancer Prevention (PDQ®)–Health Professional Version. https://doi.org/10.1038/s41572-021-00370-0 World Health Organization. (2021). Human papillomavirus (HPV) and cervical cancer. https://www.who.int/news-room/fact-sheets/detail/human-papillomavirus-(hpv)-and-cervical-cancer MedlinePlus. (2023). HPV and Pregnancy. https://medlineplus.gov/hpvpregnancy.html We know this journey can bring uncertainty. Stay calm, trust your medical team, and share your questions at every visit. If you have specific concerns or are seeking an assisted reproduction plan, consult a fertility specialist. We’re with you every step of the way!

Starting the journey to parenthood is exciting, but it can also raise questions about how to prepare. At Ingenes we guide you with a clear, approachable guide covering all aspects—physical, emotional, and lifestyle—to plan your pregnancy with confidence. First medical steps before conceiving Before trying to conceive, the most important step is to consult a fertility specialist. Together you’ll review your medical history and health status. Conditions like diabetes, hypertension, or sexually transmitted infections can affect pregnancy. A comprehensive checkup (blood tests, hormone profile, and imaging studies) will help you start off on the right foot. Nutrition and supplements A balanced diet and the right supplements are key: Folic acid: at least 400 µg daily, starting 3 months before conception. Iron: 18 mg per day. Calcium: 1,000 mg per day. Vitamin D: 600 IU per day. Choose whole grains, lean proteins, fruits, vegetables, and healthy fats. Avoid extreme diets. How to monitor fertility and ovulation Track your menstrual cycle by recording daily basal body temperature and changes in cervical mucus. Use a fertility app or calendar and consider ovulation kits (LH tests) to pinpoint your fertile window more accurately. Lifestyle and fertility Quit smoking and limit alcohol. Maintain a BMI between 18.5 and 24.9 kg/m². Do moderate exercise: 150 minutes of aerobic activity per week. Manage stress with yoga, meditation, or therapy. Review medications and medical conditions Some drugs—antidepressants, antihypertensives, anticonvulsants—can affect fertility or fetal development. Do not stop or change doses without consulting a specialist in Assisted Reproduction. Advanced reproductive options If after 6–12 months of trying (depending on age) you haven’t conceived, consider assisted reproduction. At Ingenes we offer everything from ovulation induction and IUI to IVF: A Complete Guide, always tailored to your needs. We assess sperm quality, ovarian reserve, and uterine health to recommend the best path. For more information, see our Comprehensive Guide to Reproductive Medicine. Emotional well-being with Ingenes We know trying to conceive can be an emotional roller coaster. That’s why we offer counseling, support groups, and stress-management workshops so you and your partner feel supported, informed, and empowered. Frequently Asked Questions (FAQ) How long should I take folic acid? Start at least 3 months before conception with 400 µg daily. Consult your specialist if you need higher doses (up to 4 mg/day) based on your history. Does stress affect fertility? Yes. Chronic stress alters hormones like cortisol and prolactin and can impair ovulation and sperm production. Relaxation techniques and emotional support improve your chances. When should I see a fertility specialist? Under 35: after 12 months of trying without protection. Over 35: after 6 months. If you have conditions like PCOS or endometriosis, seek help sooner. Do men get tested too? Male fertility accounts for 40–50% of cases. A semen analysis evaluates count, motility, and morphology. Depending on results, hormonal or genetic tests may be required. Sources American College of Obstetricians and Gynecologists. (2021). Practice Bulletin No. 200: Early Pregnancy Loss. Obstetrics & Gynecology, 136(4), e139–e153. https://doi.org/10.1097/AOG.0000000000004554 Centers for Disease Control and Prevention. (2022). Preconception Health and Healthcare. https://www.cdc.gov/preconception/index.html MedlinePlus. (2023). Folic Acid. https://medlineplus.gov/folicacid.html Practice Committee of the American Society for Reproductive Medicine. (2020). Diagnostic evaluation of the infertile female. Fertility and Sterility, 113(3), 545–553. https://doi.org/10.1016/j.fertnstert.2019.11.014 We’re with you every step of the way. If you have questions or want a personalized plan, consult an assisted reproduction specialist for the best care.

The Mediterranean diet is famous for its health benefits and now also for its role in fertility. If you’re starting an in vitro fertilization (IVF) treatment, take note! A diet rich in fruits, vegetables, legumes, fish, and olive oil provides key nutrients that can increase your chances of success. What is the mediterranean diet and why does it matter in IVF? It’s based on fresh, natural foods: fruits, vegetables, whole grains, legumes, nuts, fish, and extra virgin olive oil. It includes dairy and lean meats in moderate portions and limits sugars and saturated fats. This way, you get antioxidants, omega-3 fatty acids, fiber, and micronutrients that improve egg quality, embryo development, and endometrial health. How does it improve egg and embryo quality? Studies show the Mediterranean diet: Reduces oxidative stress with antioxidants (vitamins C and E). Supports mitochondrial function with omega-3 fatty acids (EPA and DHA). Promotes healthy cell division thanks to folate. Key nutrients for fertility Antioxidants: vitamins C (ascorbic acid) and E (tocopherol). Omega-3: 1–2 g/day from fish or flaxseed. Folate: 400 µg/day from leafy greens and legumes. Monounsaturated fats: 20–40 mL/day of extra virgin olive oil. Incorporate the mediterranean diet today Choose seasonal produce, use 30–40 mL of extra virgin olive oil daily, and eat fish (salmon, sardines) 2–3 times a week (150 g per serving). Swap refined grains for whole grains—quinoa, farro, or whole wheat bread—snack on a handful (30 g) of nuts or seeds, and add 100 g of cooked legumes. A healthy, sustainable lifestyle Besides improving fertility, this diet protects your heart, regulates blood sugar, and reduces the risk of certain cancers. Prioritize plant-based foods, minimize processed items, and practice mindful eating. How Ingenes supports your nutrition At Ingenes we understand that nutrition is crucial in IVF. Our team guides you with personalized plans, integrating dietary counseling and advanced reproductive techniques. Discover the secret to successful IVF. The importance of balanced nutrition A well-balanced meal plan ensures essential macro and micronutrients for healthy eggs, quality embryos, and a receptive endometrium. More details at “The Importance of Nutrition in Fertility Treatment”. Practical tips for your reproductive health Fruits and vegetables: 5 servings daily. Lean proteins: 1.2–1.5 g/kg body weight (fish, poultry, legumes). Healthy fats: 20–35% of daily calories. Hydration: 2–2.5 L of water per day. Frequently Asked Questions 1. How long until I see changes? Following the diet for 3–6 months before IVF improves oocyte and embryo quality. Antioxidant levels rise in weeks, while lipid profiles and inflammatory markers stabilize over months. Consistency and gradual changes are key to regulating hormones, maintaining stable cycles, and optimizing endometrial receptivity. 2. What if I have dietary restrictions? The Mediterranean diet is flexible. If you’re vegan or vegetarian, increase legumes (100–150 g cooked) and nuts (30 g). For omega-3, use chia seeds or algae supplements. If lactose intolerant, choose fortified plant-based milks. Always consult your specialist or a dietitian. 3. What should I avoid in IVF? Limit red meat to under 300 g/week and avoid processed foods. Reduce sweets, refined grains, caffeine (≤200 mg/day), and alcohol. Opt for whole, colorful foods. 4. Why does olive oil help implantation? Extra virgin olive oil provides oleic acid and polyphenols that improve blood flow and reduce endometrial inflammation. With 20–40 mL daily, you promote a thicker, healthier uterine lining. Sources Consulted Martínez-González, M. A., & Estruch, R. (2021). Mediterranean diet, cardiovascular disease and mortality: a critical review. European Journal of Internal Medicine, 82, 1–3. https://doi.org/10.1016/j.ejim.2020.10.004 Gaskins, A. J., & Chavarro, J. E. (2018). Diet and Fertility: a review. American Journal of Obstetrics and Gynecology, 218(4), 379–389. https://doi.org/10.1016/j.ajog.2017.11.587 National Library of Medicine. (2022). Antioxidants and Reproductive Biology. MedlinePlus. https://medlineplus.gov/antioxidantsandreproductivehealth.html Thompson, J., & Hanna, J. (2020). Omega-3 Fatty Acids in Reproductive Health. Fertility and Sterility, 114(5), 987–993. https://doi.org/10.1016/j.fertnstert.2020.07.010 We know the journey to parenthood can be challenging. You’re not alone: every step counts. If you seek guidance and support, consult a fertility specialist for a personalized, professional plan to accompany you on this journey.

Polycystic Ovary Syndrome (PCOS) is not just ovaries with cysts: it’s a hormonal imbalance that impacts your overall health, from metabolism to mood. Here you’ll learn what PCOS is, why it occurs, how it’s diagnosed, available treatments, and possible long-term effects. What is PCOS and what does it mean? PCOS commonly occurs in women of reproductive age. Its main signs are: Irregular or absent menstrual cycles Excess androgens: hirsutism, acne, hair loss Ovaries with a polycystic appearance on ultrasound Additionally, PCOS affects your insulin sensitivity, blood lipid profile, and emotional well-being. Do not self-medicate: a specialist must make a proper diagnosis. What causes PCOS and who is at risk? There’s no single cause: genetic and environmental factors play a role: Insulin resistance, which triggers androgen production Hormonal imbalance: high testosterone and LH levels Family history of PCOS If your goal is pregnancy, consult a Reproductive Medicine specialist before taking any medication. How is PCOS diagnosed? The Rotterdam criteria require two of three: Oligomenorrhea or amenorrhea Hyperandrogenism (clinical or biochemical) Polycystic ovaries on ultrasound (more than 12 follicles of 2–9 mm or volume ≥ 10 mL) Treatments to manage PCOS There’s no definitive cure, but effective management options include: Diet and exercise: losing 5–10% of body weight improves insulin sensitivity and regulates cycles Oral contraceptives and antiandrogens like spironolactone Fertility therapies: clomiphene and gonadotropins IVF and other assisted reproduction techniques: advanced options Long-term consequences Fertility: anovulation complicates conception, but with treatment many achieve pregnancy Metabolic syndrome: increased risk of type 2 diabetes, obesity, and dyslipidemia Cardiovascular system: hypertension, high cholesterol, early atherosclerosis Mental health: anxiety and depression; psychological support helps Pregnancy: higher likelihood of gestational diabetes, preeclampsia, and preterm birth PCOS is a red flag for your health: a multidisciplinary approach with nutrition, gynecology, endocrinology, and emotional support makes all the difference. FAQ: Frequently Asked Questions 1. Can it improve with lifestyle changes alone? You’ll see significant improvement with a balanced diet (high in fiber, low in refined sugars) and exercise (150 min/week). Losing 5–10% of body weight helps restore ovulation and reduce insulin resistance. Ongoing management is still required. 2. Can I get pregnant with polycystic ovaries? Yes. With ovulation induction (clomiphene, letrozole) or assisted reproduction (IVF) many women achieve pregnancy. Early diagnosis and a personalized plan are key. Do not self-medicate. 3. How does PCOS affect the heart? It increases your risk of hypertension and dyslipidemia, accelerating atherosclerosis. Monitor blood pressure, glucose, and cholesterol, and adopt healthy habits to prevent future issues. 4. What tests are required for diagnosis? Pelvic ultrasound plus tests for LH, FSH, estradiol, free testosterone, prolactin, and TSH. Also a glucose tolerance test and lipid profile. Everything is interpreted alongside your symptoms and medical history. Sources Goodarzi, M. O., et al. (2011). Polycystic ovary syndrome: Etiology, pathogenesis and diagnosis. Nature Reviews Endocrinology, 7(4), 219–231. https://doi.org/10.1038/nrendo.2010.217 Legro, R. S., et al. (2013). Diagnosis and treatment of polycystic ovary syndrome: An Endocrine Society clinical practice guideline. The Journal of Clinical Endocrinology & Metabolism, 98(12), 4565–4592. https://doi.org/10.1210/jc.2013-2350 MedlinePlus. (2023). Polycystic Ovary Syndrome. https://medlineplus.gov/polycysticovarysyndrome.html American College of Obstetricians and Gynecologists. (2018). Practice Bulletin No. 194: Polycystic Ovary Syndrome. Obstetrics & Gynecology, 132(1), e157–e173. https://doi.org/10.1097/AOG.0000000000002658 Remember that every body is unique. If you’re seeking fertility or PCOS management, consult a fertility specialist. You’re not alone on this journey!

Michelle Obama’s brave revelation about her experience with pregnancy loss has touched the hearts of millions of women around the world. Her story is not only one of pain and loss but also one of resilience and hope. By openly sharing her journey through infertility, Michelle has shed light on a topic that often remains in the shadows, surrounded by stigma and silence. At Ingenes, we recognize the importance of these personal narratives and how they can inspire and encourage other women facing similar challenges in their desire to start a family. Michelle’s tragic experience highlights an issue that affects a surprisingly large number of couples around the world. Pregnancy loss, a deeply moving and life-changing event, can leave lasting emotional scars and unanswered questions. At Ingenes, we are committed to providing a safe and supportive space where these stories can be shared and where couples can find a sense of community and understanding. Our mission at Ingenes goes beyond offering cutting-edge fertility treatments. We strive to understand the emotional and physical complexities our patients face on their path to parenthood. Michelle Obama’s story not only motivates us to continue our work, but also reminds us of the importance of approaching these issues with sensitivity, care, and a deep respect for each person’s individual experiences. What lessons can we learn from Michelle Obama’s pregnancy loss? In “Becoming”, Michelle Obama shares the intimate details of her experience with miscarriage. This honest account reminds us that pregnancy loss affects 10–20% of known pregnancies and is often underreported due to stigma. By speaking openly, she has given voice to many women who feel alone in their grief and inspired them to seek support. How does In Vitro Fertilization work and when should it be considered? After their loss, the Obamas opted for In Vitro Fertilization (IVF). IVF involves retrieving mature eggs and sperm, combining them in a lab dish, and transferring viable embryos into the uterus. Success rates vary by age and clinic but can range from 30% to 50% per cycle. At Ingenes, we tailor protocols—dosing hormones in IU and monitoring follicle growth in mm—to optimize outcomes. Why is emotional support crucial during infertility treatments? Pregnancy loss and fertility treatments carry a heavy emotional toll. At Ingenes, we complement our medical protocols with counseling services, support groups, and mind–body therapies. Studies show that women who receive psychosocial support have higher treatment adherence and report reduced anxiety and depression. Our approach is rooted in empathy: we listen, validate your feelings, and accompany you at every step. How can personalized treatment plans improve fertility outcomes? Couples respond differently to medications and protocols. By analyzing AMH levels in ng/mL, antral follicle counts, and genetic factors, our team crafts individualized plans. Whether it’s adjusting the gonadotropin dose from 150 IU to 300 IU or selecting time-lapse embryo monitoring, personalization boosts implantation rates. Michelle Obama’s story is a source of inspiration and hope. At Ingenes, we strive to provide our patients with the best fertility care and treatments, helping them turn their dreams of becoming mothers into reality. For more success stories, explore Celebrities and In Vitro Fertilization: Stories of Success and Hope. Avoid self-medicating without consulting a doctor. Before resorting to this medication, you need to see a specialist in assisted reproduction, particularly if you are looking to increase your chances of getting pregnant. Frequently Asked Questions What are the most common causes of pregnancy loss? Chromosomal abnormalities in the embryo account for nearly 50% of miscarriages, especially in the first trimester. Other factors include uterine malformations, hormonal imbalances like low progesterone, thyroid disorders, or uncontrolled diabetes. Lifestyle factors—smoking, excessive caffeine, or obesity—can also increase the risk. How long should I wait after a miscarriage before trying again? Medical guidelines suggest waiting at least one to three regular menstrual cycles before attempting conception to allow the endometrium to recover and ensure accurate dating of a new pregnancy. Emotional readiness is equally important—seek counseling if feelings of grief or anxiety persist. When is it appropriate to consider assisted reproduction? Couples under 35 who have tried unprotected intercourse for 12 months without success, or women over 35 who have tried for six months, should be evaluated for infertility. Factors like low ovarian reserve (AMH
Every year, during the last week of April, National Infertility Awareness Week is celebrated. This initiative reminds us that infertility knows no cultures, social classes, or borders: it affects women and men of all ages and backgrounds. You might know someone close who is going through this. While supporting a friend or family member in this situation can be challenging, there are simple and effective strategies to provide help empathetically and safely. What is National Infertility Awareness Week and why does it matter? National Infertility Awareness Week (NIAW) brings together healthcare professionals, patients, and advocates to spread information about a problem affecting 1 in 6 people of reproductive age worldwide. During these days, discussions cover prevention, early diagnosis, and treatment options, from lifestyle changes to assisted reproductive technologies (ART). What factors contribute to infertility? Infertility can have many causes. In women, ovulatory disorders, tubal damage, or endometriosis are common. In men, low sperm count, reduced motility, or abnormal morphology often play a key role. Additionally, habits such as smoking, having a BMI over 30 kg/m², excessive alcohol consumption, and stress also affect fertility in both sexes. How do assisted reproductive technologies improve conception rates? At Ingenes we combine advanced ART techniques with personalized care. We offer in vitro fertilization (IVF), intracytoplasmic sperm injection (ICSI), and preimplantation genetic testing (PGT). Each plan is tailored to the patient’s medical profile, optimizing success chances and reducing risks. What lifestyle changes can boost fertility naturally? Some simple adjustments make a difference. Follow a balanced diet rich in antioxidants, maintain a healthy weight (BMI between 18.5 and 24.9), engage in moderate exercise, and limit caffeine to under 200 mg daily (about two 240 ml cups of coffee). Avoid tobacco, moderate alcohol, and devote time to stress-management techniques like yoga or meditation. Why is early medical advice important? Early evaluation by a reproductive specialist allows identification of treatable causes of infertility and initiation of interventions before age becomes a limiting factor. Do not self-medicate without consulting a professional. Visiting an Assisted Reproduction specialist is key to maximizing your chances of pregnancy. At Ingenes we also offer resources and ongoing training so our patients have the information and support they need. Discover other initiatives like International Men’s Health Week: Let’s Talk About Fertility and global campaigns like World Fertility Day. How can you support someone facing infertility? Listen without judgment, offer practical help, and encourage participation in social activities. Learn about the emotional and physical impact of infertility and suggest professional support, whether through therapy, support groups, or patient networks, so no one faces this journey alone. Resources available during National Infertility Awareness Week Webinars, workshops, and social media campaigns offer up-to-date advice on prevention and treatment. Many clinics, including Ingenes, host expert Q&A sessions. Check reliable sources like WHO Infertility and national infertility associations for local events. Frequently Asked Questions 1. Does age affect fertility in women and men? Yes. In women, fertility usually declines after age 35 due to lower ovarian reserve and egg quality. In men, fertility gradually decreases from 40, affecting motility and morphology. Early evaluation helps plan timely interventions. Tests like anti-Müllerian hormone (AMH) and antral follicle count (AFC) assess ovarian reserve; semen analysis measures concentration (million/mL), motility (%), and morphology (% normal forms). 2. What is the success rate of IVF treatments? It depends on age, diagnosis, and clinic protocol. On average, women under 35 achieve live birth rates of 45–55% per cycle; in women over 40, rates drop to 15–20%. Factors like egg quality and embryo grading also influence outcomes. Technologies such as time-lapse and PGT help select viable embryos, improving results. Talk to your specialist for your personalized prognosis. 3. Are there non-medical methods to increase fertility? Lifestyle changes can support reproductive health: Mediterranean diet, healthy weight, less caffeine, quitting smoking, and stress management with mindfulness. Supplements like folic acid (400 µg/day) and vitamin D (600–800 IU/day) are helpful, but always avoid self-medication without consulting a doctor. 4. When should a couple seek medical advice? If they are under 35, after 12 months of unprotected intercourse without pregnancy; if over 35, after six months. Additionally, it’s advisable to seek help earlier if there are irregular cycles, severe endometriosis, or a history of pelvic infections. Early intervention detects issues like polycystic ovary syndrome (PCOS) or male factors, improving prospects by starting appropriate treatment. Sources Consulted World Health Organization. (2023). Infertility. Retrieved from https://www.who.int/health-topics/infertility Practice Committee of the American Society for Reproductive Medicine. (2020). Definitions of infertility and recurrent pregnancy loss: a committee opinion. Fertility and Sterility, 113(1), 19–25. https://doi.org/10.1016/j.fertnstert.2019.06.005 Centers for Disease Control and Prevention. (2022). Assisted Reproductive Technology (ART). Retrieved from https://www.cdc.gov/art MedlinePlus. (2023). Fertility. Retrieved from https://medlineplus.gov/fertility.html We know this journey can be difficult, but you are not alone. Seek the support of those who understand you and remember that an assisted reproduction specialist can offer the guidance and support you need to increase your chances of becoming a parent.

Nutrition and fertility are closely linked. Foods provide essential nutrients that directly influence the reproductive health of men and women. Today, our diet contains many toxins that can affect the body. Reviewing our eating habits is key, as an unbalanced diet can disrupt our biological clock. Additionally, numerous studies show that both obesity and underweight complicate conception and pregnancy. That is why fertility specialists advise following the most balanced diet possible. Why is nutrition important in fertility treatment and how does it influence conception? Many difficulties in conceiving are related to poor eating habits, so taking care of the diet is essential. Overweight women often experience ovulation disorders, and in men infertility is often linked to oligospermia (low sperm count) or poor motility. A lack of nutrients such as folic acid, zinc, and antioxidants directly affects egg and sperm quality. The World Health Organization (WHO) states that a balanced diet improves maternal and fetal health, strengthens the immune system, supports safer pregnancies and deliveries, and reduces the risk of chronic diseases such as diabetes and heart disease. Learn more about the importance of nutrition in fertility treatment to understand how proper eating can increase success rates. How to improve nutrition during fertility treatment? First, consult a nutritionist to design a personalized meal plan that fits your lifestyle and reproductive goals. If you have already started assisted reproduction, discuss dietary adjustments with your fertility specialist to optimize results. Avoid self-medication: before taking supplements or medications, always see a reproductive medicine expert. Prioritize whole foods rich in folic acid (400 µg/day), zinc (8–11 mg/day), omega-3 fatty acids (at least 250 mg of DHA+EPA/day), antioxidants (vitamins C and E), and iron (15–18 mg/day). Maintain a balanced energy intake (1,800–2,200 kcal/day for women) and drink about 2 L of water daily. WHO recommendations to support fertility The WHO advises: Follow a varied diet with fruits and vegetables to ensure essential vitamins, minerals, and antioxidants for reproductive health. Adjust caloric intake to maintain a body mass index (BMI between 18.5 and 24.9 kg/m²), as both overweight and undernutrition affect fertility in both sexes. Avoid ultraprocessed foods containing pesticides, preservatives, or endocrine disruptors that harm ovulation and sperm production. Limit alcohol, caffeine (200 mg/day), artificial sweeteners, and ultraprocessed foods with trans fats. These can disrupt hormonal balance and egg quality. Opt for whole grains, lean proteins, fresh fruits and vegetables, and healthy fats. A balanced, nutrient-rich diet creates an optimal environment for conception. Sources World Health Organization. (2021). Nutrition. https://www.who.int/health-topics/nutrition#tab=tab_1 Centers for Disease Control and Prevention. (2020). Preconception Health. https://www.cdc.gov/preconception/index.html Mayo Clinic. (2019). Nutrition and Fertility. https://doi.org/10.1016/j.fertnstert.2018.05.041 MedlinePlus. (2021). Vitamins for Pregnancy. https://medlineplus.gov/vitaminsformenstruationandfertility.html Remember that every body is unique. Stay positive and consult a fertility specialist to receive proper guidance and increase your chances of success.

Understanding the fertilization process is essential when you’re trying to conceive. Although fertilization is an amazing phenomenon, it happens microscopically and almost always remains unnoticed. We explain it clearly and in a friendly way. What is an egg and how does fertilization occur? The egg, or female gamete, is the cell produced by the ovaries. Each month, one of your ovaries releases an egg during ovulation and it travels through the fallopian tube toward the uterus. Fertilization occurs when a sperm penetrates the egg. Although millions of sperm make that journey, only one fuses with the egg membrane and forms the zygote. What happens at the moment of fertilization? When the sperm enters, its genetic material combines with the egg’s DNA and the zygote is formed, with 46 chromosomes (23 from each parent). In the following days, the zygote begins to divide and becomes a blastocyst, which is ready to implant in the uterus after 5–6 days. Are there symptoms when the egg is fertilized? Most women don’t feel anything at the exact moment of fertilization: it occurs in the fallopian tube at a cellular level. About 6–10 days later, when the blastocyst attaches to the uterus, you may experience light spotting or mild cramps. Every body is different, and these signs don’t guarantee success 100%. How does the fertilized egg travel and implant? It takes the zygote 6–10 days to reach the uterus. During this journey it divides and by day five it becomes a blastocyst which, upon finding a prepared endometrium, embeds itself in its lining: implantation. Factors influencing fertilization success Egg and sperm quality, timing of intercourse or insemination, health of the tubes and uterus, and age (better quality before 35) play decisive roles. In addition, good nutrition, stress management, and avoiding tobacco improve your chances. A fertility specialist can guide you every step of the way, and if you need support, our patient care services are here for you. Frequently Asked Questions 1. Can you feel fertilization when it happens? No. It’s a cellular process inside the fallopian tube. If you notice discomfort days later, it’s usually due to implantation, not fertilization itself. 2. Ovulation pain vs. implantation cramping? Mittelschmerz occurs at ovulation (day 14 in a 28-day cycle) and lasts minutes or hours. Implantation cramps appear 6–10 days after fertilization and often come with light spotting. 3. Does implantation bleeding mean pregnancy? It can be an early indication, but not everyone experiences it. If it appears before your period, very light and brief, it could be implantation. To confirm, take a pregnancy test after your missed period or consult your doctor. 4. When should you see a specialist? If you’ve been trying to conceive for 6–12 months without success (depending on your age), or have irregular cycles, severe menstrual pain, or a complicated reproductive history, seek professional advice. We’re with you on this journey. Every body is unique and sometimes we need extra support. Don’t hesitate to consult a reproductive medicine specialist for the guidance and care you deserve.

Implantation failure is diagnosed when, after at least three cycles of in vitro fertilization or the transfer of more than ten good-quality embryos, pregnancy is not achieved. Today we have highly effective solutions for every cause of implantation failure: blastocyst‐stage transfer (day 5), preimplantation genetic testing for aneuploidy (PGT-A) and assisted hatching. What is implantation failure and why is it important to identify? Embryo implantation requires a good-quality embryo, a receptive endometrium and effective communication between both. When pregnancy is not achieved after three IVF cycles or more than ten embryos transferred, it is called implantation failure. Early detection guides treatment and improves your chances of success. Most common causes Embryonic: chromosomal abnormalities or difficulty hatching from the zona pellucida. Uterine: malformations, fibroids, adhesions, synechiae, endometritis or hydrosalpinx. Hormonal or metabolic: antiphospholipid syndrome, insulin resistance or obesity. Thrombophilias: clotting disorders. How it is diagnosed Blood tests: hormones, metabolic profile, immunological markers and coagulation tests. Transvaginal ultrasound: identifies fibroids or malformations, measures endometrium (ideal ≥ 7 mm) and evaluates hydrosalpinx. Sperm DNA fragmentation: complements semen analysis if genetic damage is suspected. PGT-A: detects aneuploidies and selects euploid embryos. Zona pellucida monitoring: after culture to blastocyst to assess assisted hatching. Reviewing your cycle history (oocyte yield, fertilization, embryo quality) helps personalize prognosis. Treatment options Immunological: specific medication under medical supervision. Uterine: from hormonal therapies to minimally invasive procedures. Embryonic: cutting‐edge techniques: Blastocyst transfer Culturing embryos to day 5–6 allows selection of those with the highest implantation potential. Preimplantation Genetic Testing (PGT-A) By transferring only euploid embryos, you reduce the risk of failure and pregnancy loss, regardless of maternal age. This accelerates the path to pregnancy. Assisted hatching A laser creates a controlled opening in the zona pellucida to facilitate blastocyst–endometrium contact. For more details, see Implantation Failures: Understanding the Challenge. Frequently Asked Questions (FAQ) How Does Maternal Age Affect It? With age, oocyte quality declines and aneuploidy risk increases, making implantation harder. That’s why PGT-A is often recommended after age 35. But each case is unique: immunological, uterine and lifestyle factors also matter. Why Does Endometrial Thickness Matter? An endometrium ≥ 7 mm is associated with better receptivity. But vascularization and the implantation window also count. Specific tests help determine the ideal transfer timing. Is Assisted Hatching Safe? Yes, when performed by trained personnel using advanced laser. It takes seconds and, when done correctly, does not harm the embryo. It is recommended after previous failures and for blastocysts with thickened zona pellucida. Why Shouldn’t I Self-Medicate? Each hormone therapy or immunomodulator requires precise dosing and monitoring. Self-medication can create unnecessary risks. Sources Practice Committee of the American Society for Reproductive Medicine. (2020). Evaluation and treatment of recurrent implantation failure: a committee opinion. Fertility and Sterility, 113(2), 278–285. MedlinePlus. (2023). IVF. https://medlineplus.gov/ivf.html American College of Obstetricians and Gynecologists. (2021). Assessment and treatment of recurrent pregnancy loss. ACOG Practice Bulletin, 225. ESHRE Recurrent Implantation Failure Working Group. (2019). Definitions and diagnosis of recurrent implantation failure: a consensus statement. Human Reproduction, 34(10), 215–226. We know this journey can be challenging, but you are not alone. Every story is unique and deserves a tailored plan. If you suspect implantation failure, consult a reproductive specialist: together you will increase your chances of success.
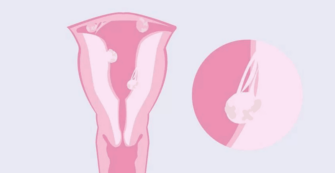
For many couples, becoming a mother or father is one of life’s most exciting and rewarding moments. But when fertility issues arise, that dream can feel increasingly distant. A common cause of infertility in women is pelvic adhesions, also called scar tissue. They develop after abdominal or pelvic surgeries, infections, endometriosis, or trauma in the area, and can hinder both conception and proper pregnancy development. In this article we explore what pelvic adhesions are and how they affect fertility. What are pelvic adhesions and why do they form? Pelvic adhesions are bands of scar tissue that bind organs—ovaries, tubes, uterus, bladder, and intestines—causing loss of mobility and normal function. They form when the body repairs inflammation or injury after surgery, infection, or endometriosis. Ovaries can become stuck to other structures, making egg release difficult. Blockage or distortion of the tubes prevents the egg and sperm from meeting. The risk of ectopic pregnancy increases if the tubes are compromised. Pain during intercourse can lead to avoiding it during fertile days. How do pelvic adhesions affect fertility and pregnancy? They interfere with gamete transport, tubal patency, and embryo migration. If the tubes are blocked or twisted, sperm cannot reach the egg, and the embryo cannot implant properly in the uterus. They also increase the risk of ectopic pregnancy (learn more about ectopic pregnancies). Assisted reproduction techniques, such as IVF, bypass these issues by retrieving eggs directly from the ovaries and transferring healthy embryos to the uterus. What symptoms may suggest the presence of adhesions? Chronic pelvic pain Very painful periods Pain during sex Difficulty conceiving Sometimes intestinal obstruction Higher risk of ectopic pregnancy Risk factors for pelvic adhesions C-section or ovarian cyst removal Myomectomy (fibroid removal) Endometriosis surgery (What is endometriosis and how does it affect fertility?) Appendicitis or pelvic inflammatory disease (from STIs like chlamydia) Infections such as hydrosalpinx Between 60% and 90% of women who undergo gynecological surgeries develop adhesions. Laparoscopy reduces the risk but does not eliminate it. Pelvic adhesions How are adhesions safely diagnosed? Laparoscopy is the gold-standard test but can create new adhesions. At Ingenes we prefer a non-invasive transvaginal ultrasound (TVUS) first and sometimes a hysterosalpingography (HSG) with contrast (10–20 mL), which only causes mild discomfort. Treatments to conceive with pelvic adhesions IVF is the most effective option since it bypasses the tubes. Eggs are retrieved from the ovaries, fertilized in the lab, and the highest-quality embryos are transferred to the uterus, increasing pregnancy chances. Do not self-medicate: always consult a fertility specialist to design a personalized plan that maximizes your chances. What to do if you suspect you have pelvic adhesions? See a reproductive endocrinologist for a comprehensive evaluation. With your medical history, imaging tests, and personalized advice, you can choose the most appropriate treatment. At Ingenes, we support you with empathy and professionalism every step of the way toward motherhood or fatherhood. Remember to always consult a specialist before making any decisions or starting any treatment. Frequently Asked Questions 1. Can pelvic physiotherapy prevent or treat adhesions? Specialized pelvic physiotherapy improves circulation and tissue mobility, relieving pain and stiffness, but does not eliminate fibrosis. It is usually combined with medical treatments under specialist supervision. 2. Is laparoscopy safe for treating adhesions if I want to get pregnant? Laparoscopy minimizes risk compared to open surgery, using 5–10 mm incisions. However, there is still a chance of forming new adhesions. Your doctor will weigh benefits and risks based on your history and reproductive goals. 3. How long should I wait after surgery before trying to conceive? It is recommended to wait between 3 and 6 months for tissues to regenerate and inflammation to subside, although the exact time depends on the type of surgery and your recovery. Always follow your specialist’s guidance. 4. What is the success rate of IVF in women with pelvic adhesions? It depends on factors such as age, egg quality, and severity of adhesions. Generally, women under 35 can achieve over a 50% chance of clinical pregnancy per cycle. A personalized assessment will provide more precise figures. References American Society for Reproductive Medicine. Adhesion Prevention and Management. Fertility and Sterility, 113(2), 443–455 (2020). MedlinePlus. Pelvic Adhesions. U.S. National Library of Medicine (2023). Chapron C., Souza C., Gonzalez F. Adhesion Formation After Endometriosis Surgery: A Multicenter Trial. Journal of Minimally Invasive Gynecology, 25(5), 805–812 (2018). Stratton P., MacLean A. Pelvic Adhesions: Impact on Fertility and Role of Laparoscopy. Human Reproduction Update, 25(4), 457–471 (2019).

Ovarian cancer is one of the toughest health challenges women of reproductive age can face. Beyond fighting the disease, many immediately wonder how to protect their desire to become mothers. Here we clearly explore how ovarian cancer can influence fertility and what paths exist to preserve the hope of having children. We will look in detail at what ovarian cancer is, how it is detected, how its treatments can affect you, and what preservation and parenthood options are available before and after. A personalized and humane approach can make all the difference. What is ovarian cancer and how is it diagnosed? It occurs when ovarian cells grow uncontrollably. The most common type is high-grade serous carcinoma. Early detection is difficult because symptoms are mild or mistaken for other ailments. Some risk factors include: Age over 50 Family history of ovarian or breast cancer BRCA1 or BRCA2 genetic mutations Endometriosis Never having had children But it can occur in younger women, raising concerns about future fertility. How does ovarian cancer treatment affect fertility? These treatments can damage your ability to conceive: Surgery: Sometimes one or both ovaries and/or fallopian tubes must be removed. Chemotherapy and radiotherapy: Can damage the ovaries and cause premature ovarian failure. Hormonal disruption: May halt ovarian function sooner than expected. Each case is different depending on cancer stage, treatment, and your motherhood plans. What fertility preservation options are available before treatment? When the diagnosis allows, it is possible to freeze eggs, embryos, or ovarian tissue before starting cancer treatment. 1. Egg freezing The ovary is stimulated to retrieve multiple eggs, which are then vitrified for future use. Advantages: You preserve your own eggs. Ideal for young women without a partner or who prefer to postpone fertilization. 2. Embryo freezing If you have a partner or accept donor sperm, eggs are fertilized and embryos are frozen. Advantages: High survival rate and viability of embryos. 3. Ovarian tissue preservation Experimental technique: tissue is removed and frozen for reimplantation after treatment. Advantages: Quick when there’s no time for stimulation. Disadvantages: Less available and still under study. Parenthood options after treatment If you couldn’t preserve or your ovaries were damaged, there are still alternatives: 1. Donor eggs IVF is performed with a donor’s eggs and sperm from your partner or a donor. 2. Surrogacy If your uterus cannot carry a pregnancy or there is a risk of recurrence, another woman carries the pregnancy. 3. Adoption It is a legal, loving option to create your family. Medical and emotional factors post-cancer When to try pregnancy: Generally recommended to wait 2 to 5 years after treatment. Medical follow-up: Ultrasounds, hormone tests, and tumor markers ensure safety. Psychological support: Essential to manage the emotional process. Why choose a specialized center? A team expert in assisted reproduction, like Ingenes, offers: Ovarian reserve assessment Egg or embryo freezing before treatment Personalized IVF programs Genetic counseling for BRCA mutations Continuous emotional support Key questions for your doctor How will my treatment affect my fertility? Can I delay treatment to preserve eggs or embryos? Which preservation method is best for me? How long should I wait before trying to conceive? How does my genetics influence my reproductive plans? Do not self-medicate without professional advice. Every decision impacts your health and your chances of becoming a parent. Rely on assisted reproduction experts to answer your questions and map the path that best fits your situation. You are not alone on this journey!

Polycystic Ovary Syndrome (PCOS) accompanies many women beyond their fertile years and often has a familial basis. Here we explain its symptoms and how it manifests at each stage of life. At what age can PCOS be detected in girls? Before age 11 and without having had their first period, a PCOS diagnosis is uncommon. From age 11 onward, a specialist can assess early signs, although before menarche there aren’t always menstrual irregularities. PCOS symptoms during adolescence Illustration of ovaries with PCOS During adolescence, PCOS signs can be mistaken for normal puberty changes. Watch for: Irregular cycles: amenorrhea or oligomenorrhea Acne or skin blemishes Excess hair growth or hair loss Muscle development with smaller breasts Precocious puberty before ages 8–9 PCOS in early adulthood Claudia, an Ingenes mom living with PCOS Between ages 20 and 30, PCOS is the most common endocrine disorder and can hinder conception. A healthy diet, regular exercise, and maintaining an appropriate weight help balance hormones and support ovulation. PCOS and menopause Although large studies are lacking, women with long-term PCOS have a higher risk of cardiovascular disease and type 2 diabetes due to elevated testosterone levels and insulin resistance. Can you conceive with PCOS? Claudia on her delivery day Consult your gynecologist and fertility specialist to design a personalized assisted reproduction plan. Options include: Ovulation induction and timed intercourse Using Clomiphene (Omnifin or others) to stimulate ovulation while avoiding hyperstimulation through monitoring. Combined with Timed Intercourse, intercourse is synchronized with ovulation. Ideal if you’re under 35 with no other factors. When to recommend in vitro fertilization? If induction is unsuccessful, your specialist may suggest up to 4 IVF cycles. Eggs are retrieved, fertilized in the lab, and the best embryos are transferred. Success rates depend on age, egg quality, and embryo selection. At Ingenes, with our Initial Program you’ll receive a complete fertility assessment and a personalized treatment plan. Start planning your life with your baby today. Read “My Pregnancy with Polycystic Ovary at Age 36” and discover success stories. To learn more about PCOS visit “PCOS: What You Should Know to Have Your Baby”. Frequently asked questions PCOS diagnosis in adolescents Clinical evaluation, ultrasound, and hormonal tests (LH, FSH, testosterone, insulin) are combined. Ultrasound can show multiple small follicles (2–9 mm) in the ovary. Early diagnosis allows lifestyle adjustments to reduce insulin resistance and regulate menstruation. What lifestyle changes help? A balanced diet low in simple sugars and high in fiber controls insulin. Aerobic exercise (30 min, 5 times/week) supports weight management and reduces androgens. Stress management techniques like yoga or meditation improve hormonal balance. Always consult your doctor before taking supplements or starting restrictive diets. Can women over 35 with PCOS conceive naturally? Ovarian reserve declines with age, but natural conception is possible if cycles are regular and lifestyle is healthy. Weight loss in overweight women can restore ovulation. If irregularity persists after 6–12 months of trying, seek expert help to increase your chances. Long-term risks of PCOS PCOS increases the risk of type 2 diabetes, cardiovascular diseases, and endometrial cancer due to chronic anovulation and hyperinsulinemia. Regular checks of glucose tolerance, lipid profile, and blood pressure are key. Hormonal treatments and metformin can reduce these risks. Sources American College of Obstetricians and Gynecologists. (2021). Practice Bulletin No. 194: Polycystic Ovary Syndrome. Obstetrics & Gynecology, 137(2), e1–e19. https://doi.org/10.1097/AOG.0000000000004255 MedlinePlus. (2023). Polycystic Ovary Syndrome. U.S. National Library of Medicine. https://medlineplus.gov/pcos.html Fauser, B. C., Tarlatzis, B. C., Rebar, R. W., Legro, R. S., Balen, A. H., Lobo, R., et al. (2012). Consensus on Women’s Health Aspects of Polycystic Ovary Syndrome (PCOS). Fertility and Sterility, 97(1), 28–38. https://doi.org/10.1016/j.fertnstert.2011.09.024 Legro, R. S., Arslanian, S. A., Ehrmann, D. A., Hoeger, K. M., Murad, M. H., Pasquali, R., et al. (2013). Diagnosis and Treatment of Polycystic Ovary Syndrome: An Endocrine Society Guideline. The Journal of Clinical Endocrinology & Metabolism, 98(12), 4565–4592. https://doi.org/10.1210/jc.2013-2350 Remember: every body is different. Stay informed, take care of your health, and seek the guidance of an assisted reproduction specialist to turn your desire to become a parent into reality.

Argentine singer María Becerra, 25, recently suffered another ectopic pregnancy. Sharing her experience helps break the stigma: this condition can affect women and men at any stage of life. At Ingenes we support you with medical and emotional care. Discover what an ectopic pregnancy is, why it can recur, and what your options are. What is an ectopic pregnancy and how does it happen? An ectopic pregnancy occurs when the fertilized egg implants outside the uterus, usually in the fallopian tubes. It affects 1 in 50 pregnancies and, if not identified in time, can be life-threatening. Never self-medicate; early diagnosis includes transvaginal ultrasound and blood hCG measurement (mIU/mL). What are the risk factors for recurrence? If you’ve had an ectopic pregnancy before, the risk of it happening again rises to 10–15%. Other factors: pelvic infections, tubal surgeries, and anatomical abnormalities. Before choosing a treatment, consult a reproductive specialist to increase your chances of a healthy pregnancy. How does it affect you emotionally and what support is available? The psychological impact can be as strong as the physical: grief, anxiety, and fear of another loss are common reactions. In Ectopic Pregnancy: Can I Have Children After This? you’ll find success rates and follow-up options for tubal function. At Ingenes we have psychologists and assisted reproduction specialists offering cognitive-behavioral therapy and support groups. Helena’s story, who overcame endometriosis with professional support, shows that resilience and proper care make a difference. What medical treatments exist and when to consider them? Options include methotrexate (50 mg/m² IM) or laparoscopic surgery. The decision depends on the size of the ectopic mass, hCG levels, and your hemodynamic stability. In case of hemoperitoneum or severe abdominal pain, surgery is prioritized. After treatment, hCG is monitored every 48 hours until levels drop below 5 mIU/mL. It’s recommended to wait 3–6 months before trying for a new pregnancy to reduce risks. Importance of early detection Recognize symptoms such as severe abdominal pain, abnormal vaginal bleeding, or dizziness and see a doctor without delay. Recommendations for emotional care Sharing your experience with professionals and support groups eases the emotional burden. Don’t isolate yourself and ask your doctor for mental health resources. Frequently Asked Questions 1. Can I get pregnant after an ectopic pregnancy? Yes. More than 65% of patients achieve an intrauterine pregnancy within 18 months after treatment. The prognosis depends on tubal function and the type of intervention received. Check success rates and make a plan with your specialist. 2. How long should I wait to try again? Usually 3–6 months, during which your hCG levels normalize and your body recovers. Your doctor will assess your overall health, ovarian reserve (AMH in ng/mL), and recurrence risk before giving you the green light. 3. What care should I take after treatment? Monitor your hCG levels until they are undetectable (< 5 mIU/mL). Follow rest recommendations, avoid intense exercise, and maintain a balanced diet with at least 1.0 g/kg of protein daily to support healing. Attend all follow-up appointments: ultrasound confirms resolution and rules out complications. 4. How to manage the psychological impact? Talking to a specialized psychologist reduces the risk of anxiety and depression. Group therapy provides practical tools and emotional support. At Ingenes we offer individual and group sessions to help you regain confidence in your body. Sources consulted American College of Obstetricians and Gynecologists. (2021). Ectopic Pregnancy. https://doi.org/10.1097/AOG.0000000000004617 MedlinePlus. (2023). Ectopic pregnancy. https://medlineplus.gov/ectopicpregnancy.html Practice Committee of the American Society for Reproductive Medicine. (2020). Medical treatment of ectopic pregnancy: A committee opinion. Fertility and Sterility, 114(5), 993-1003. https://doi.org/10.1016/j.fertnstert.2020.07.001 World Health Organization. (2018). Safe abortion: Technical and policy guidance for health systems. https://apps.who.int/iris/handle/10665/70914 We want you to know that you are not alone on this journey. Every story is unique and your well-being matters. If you suspect you have an ectopic pregnancy or seek guidance for your next steps, consult a specialist in assisted reproduction. We are here to support you.

Hyperprolactinemia occurs when blood prolactin levels exceed 25 ng/mL in someone who is neither pregnant nor breastfeeding. This hormone, produced by the pituitary gland, is key for breast development and lactation. Outside of pregnancy, elevated levels disrupt GnRH signaling, halt ovulation, disturb menstruation, and lower estrogen, complicating conception. In women and men, excess prolactin may present with: Absent or irregular menstruation (amenorrhea, oligomenorrhea) Milk production without breastfeeding (galactorrhea) Anovulation and infertility Frontal or retro‐ocular headaches and visual disturbances Decreased libido Hirsutism if associated with PCOS Recurrent pregnancy losses What causes hyperprolactinemia? Physiological: pregnancy, lactation, stress, intense exercise, sleep deprivation. Systemic: hypothyroidism, chronic renal failure, cirrhosis, lupus, multiple sclerosis. Medications: antipsychotics, metoclopramide, estrogens, calcium channel blockers. Pituitary adenomas: prolactinomas (micro <10 mm or macro >10 mm). Diagnosis Measure fasting prolactin after 30 minutes of rest; repeat if elevated. Exclude pregnancy and medications that raise prolactin. Evaluate TSH to rule out hypothyroidism. If persistent, perform pituitary MRI or CT scan. Do not self‐medicate: always consult a reproductive medicine specialist. Treatment and pathway to pregnancy Discontinue or switch causative medications under medical supervision. Treat hypothyroidism with thyroid hormone. Dopamine agonists (bromocriptine or cabergoline): start low and adjust until prolactin <20 ng/mL; ovulation and menstruation usually resume in 2–3 months. If no response after 6 months or macroadenoma >10 mm: transsphenoidal surgery or radiotherapy. If anovulation persists, complement with in vitro fertilization (IVF) to retrieve and fertilize eggs directly. Frequently Asked Questions 1. Can mild prolactin elevation normalize on its own? Moderate elevations (20–40 ng/mL) may correct with less stress and better sleep, but require lab follow‐up and specialist evaluation. If it lasts more than 3 months or symptoms occur, treatment is needed. 2. When do I see results with dopamine agonists? Ovarian function and menstruation improve in 2–3 months. Treatment starts with bromocriptine 1.25 mg/day or cabergoline 0.25 mg/week and is adjusted based on response. 3. Do these treatments affect my health? Dopaminergic agonists can cause nausea, dizziness, or headache, but these are usually temporary. Thyroid hormone therapy improves energy and overall well‐being. 4. Does high prolactin increase miscarriage risk? Yes. Elevated prolactin can impair implantation and luteal function. Treating it reduces early losses and improves chances of pregnancy. We understand how important this journey is: seeking emotional support, managing stress, and working with a reproductive medicine team makes a difference. Consult a professional to evaluate your case and guide you toward the pregnancy you desire.

Every May 28 we celebrate Nutrition Day, a perfect date to reflect on how diet influences our health and, especially, our fertility. Although we often associate nutrition with weight or energy, few know that a balanced diet is key to increasing your chances of pregnancy. In this article we explain how a proper diet can support fertility, why at Ingenes we place so much importance on this aspect, and what changes you can adopt if you’re trying to have a baby. Why is nutrition essential for fertility? Fertility doesn’t depend solely on reproductive organs. Hormonal balance, cellular function, and metabolism are fueled by what we eat. A diet lacking vitamins and minerals can cause polycystic ovary syndrome (PCOS), ovulation disorders, or premature ovarian insufficiency in women, and in men it can affect sperm count, motility, and morphology. At Ingenes we assess your eating habits before any treatment and design a personalized plan to optimize hormone production, egg maturation, and uterine receptivity. Key nutrients to improve your fertility 1. Folic acid (400–800 µg/day) Essential for DNA synthesis and cell division. In women it improves egg quality and neural tube development; in men it increases sperm count and motility. Sources: spinach, lentils, broccoli, avocado, fortified cereals. 2. Zinc (8–12 mg/day) Regulates menstrual cycles and testosterone levels. In men it’s key for spermatogenesis. Sources: lean meats, seafood, pumpkin seeds, nuts. 3. Omega-3 (1–2 g/day) Its anti-inflammatory properties improve uterine blood flow and embryo implantation. In men it enhances sperm motility and membrane fluidity. Sources: salmon, sardines, flaxseed, walnuts. 4. Iron (18 mg/day women; 8 mg/day men) Prevents anemia and supports ovulatory function. Sources: red meat, legumes, spinach, fortified whole grains. 5. Antioxidants (Vitamin C 75 mg/day; Vitamin E 15 mg/day; Selenium 55 µg/day) Protect germ cells from oxidative stress. Sources: citrus fruits, berries, peppers, almonds, sunflower seeds. How does a poor diet affect fertility treatments? A diet high in refined sugars, trans fats, and ultraprocessed foods can: Increase insulin resistance (linked to PCOS). Disrupt ovulation and cycle regularity. Raise chronic inflammation. Reduce sperm DNA integrity. Hinder endometrial receptivity. These metabolic imbalances lower success rates in in vitro fertilization (IVF) and intrauterine insemination (IUI). Which diet supports assisted reproduction treatments? We recommend a Mediterranean-style diet: fruits, vegetables, whole grains, lean proteins, and healthy fats. This pattern has shown: Better ovarian response. Higher quality eggs and embryos. Increased implantation rates. At Ingenes we create personalized nutrition plans based on clinical data and your lifestyle. Learn more about the importance of nutrition in your fertility treatment. Adaptations for PCOS, endometriosis, or thyroid conditions PCOS Choose low glycemic carbs, high-fiber foods, and lean proteins to control insulin. Avoid sugary drinks and refined flours. Endometriosis Include anti-inflammatory foods like fatty fish, turmeric, and leafy greens. Reduce red meat and ultraprocessed foods that may increase inflammation. Hypothyroidism Ensure adequate iodine, selenium, and vitamin D. Cook goitrogenic foods (raw broccoli, soy) well and maintain regular meal schedules. Male nutrition matters too Up to 40% of infertility causes involve male factors. A diet rich in antioxidants, lean proteins, and omega-3 improves: Sperm count, motility, and morphology. DNA integrity. Hormonal balance. Avoid alcohol, tobacco, processed meats, and excess caffeine. Nutrition services at Ingenes Individual assessments with fertility nutritionists. Diet plans for PCOS, low ovarian reserve, or autoimmune conditions. Multidisciplinary coordination with gynecology, reproductive biology, and psychology. Supplementation guidance before IVF, IUI, vitrification, or egg donation. Discover how tailored nutrition boosts your treatment at Ingenes. Celebrate Nutrition Day and nurture your fertility May 28 is a reminder to feed your body with intention. Simple changes—swap soda for water, add berries to your breakfast, or choose grilled fish instead of fried—can make a difference in your reproductive health. Remember, no advice replaces a specialist’s opinion. If you want to increase your chances of pregnancy, consult an assisted reproduction expert. We’re with you on this journey and we believe in you!

To understand how hypothyroidism influences fertility, first you need to know that the thyroid gland produces two key metabolic hormones: T4 (thyroxine) and T3 (triiodothyronine). This butterfly-shaped gland is located at the front of the neck, just below the Adam’s apple. Although there are many thyroid conditions, in this article we will focus on hypothyroidism and its impact on female fertility. Thyroid gland in the human body What is hypothyroidism and how does it affect fertility? Hypothyroidism occurs when the thyroid does not produce enough T3 and T4. In women it can disrupt ovulation, cause irregular menstrual cycles, and complicate conception. Do not self-medicate: before taking any medication, consult a Reproductive Medicine specialist. They will evaluate your case and increase your chances of pregnancy. Key symptoms in women trying to conceive Extreme fatigue Unexplained weight gain Cold intolerance Dry skin and brittle hair Irregular or absent menstrual cycles Mild depression or persistent constipation If you notice any of these changes, share them with your doctor. Recurrent miscarriages or difficulty conceiving can be warning signs. Most common causes of hypothyroidism Autoimmune thyroiditis (Hashimoto’s) Radiation therapy to the head or neck Thyroid surgery Iodine deficiency Medications (lithium, amiodarone) Pituitary disorders affecting TSH In many cases the cause is not identified, so early diagnosis is vital. Diagnosis before trying to conceive The endocrinologist will measure your neck, skin, weight, and heart rate. Then they will order a blood test to measure TSH. A value above 3.5 mU/L suggests hypothyroidism. Free T3 and T4 may also be measured to assess severity. With this data, your doctor will design a treatment plan to protect your health and that of your future baby. Treatment options if you plan to have a baby The standard treatment is levothyroxine, adjusted according to your weight (approx. 1.6 μg/kg per day) and lab results. Every body is unique: consult a Reproductive Medicine specialist to determine your dose and monitor your hormone levels. For more information, check our article Hypothyroidism and Fertility or explore Hyperthyroidism and Fertility. Ingenes family who overcame thyroid issues Frequently asked questions 1. Does hypothyroidism cause irreversible infertility? With treatment and TSH control, most patients regain ovarian function and can conceive naturally or with assisted reproduction techniques. 2. How do TSH levels influence embryonic development? TSH regulates T3 and T4, essential for ovarian follicle maturation and a receptive endometrium. Keeping TSH between 0.5–3.5 mU/L improves implantation and reduces miscarriage risk. 3. Can I improve my thyroid with diet? Include iodine (fish, seaweed, dairy), selenium (nuts), and zinc (lean meats). Avoid excessive raw goitrogenic foods like soy and broccoli. Always consult your nutritionist or endocrinologist before changing your diet. 4. Is levothyroxine treatment safe during pregnancy? Yes. Levothyroxine is the treatment of choice: it does not actively cross the placenta and ensures adequate hormone levels. During pregnancy, your dose may be adjusted; monitor TSH every 4–6 weeks. Sources Consulted American Thyroid Association. (2017). Guidelines for diagnosis and management of hypothyroidism. Thyroid, 27(3), 315-389. MedlinePlus. (2022). Hypothyroidism. https://medlineplus.gov/hypothyroidism.html de Groot et al. (2012). Management of thyroid dysfunction during pregnancy. J Clin Endocrinol Metab, 97(8), 2543-2565. Stagnaro-Green et al. (2011). Clinical practice guideline: thyroid disease in pregnancy. Thyroid, 21(10), 1081-1125. Remember that every case is unique. We are with you on this journey and encourage you to consult a fertility specialist for the personalized guidance you deserve.
In the realm of family and career planning, egg freezing is an increasingly valued option for those who wish to postpone parenthood without giving up the possibility of having children in the future. At Ingenes, we offer this cutting-edge procedure so you can approach the timing of starting your family with confidence. What is egg freezing and what is it for? Egg freezing, or oocyte cryopreservation, allows you to store your eggs at –196 °C via vitrification, ensuring they maintain their quality and reproductive potential when you decide to use them. Who are ideal candidates for egg freezing? Women who want to focus on their careers or personal projects before becoming mothers. Those who prefer to wait to find the right partner. Anyone undergoing medical treatments (such as chemotherapy) that could affect fertility. Women concerned about the natural decline in egg quality with age. What is the process at Ingenes? Ovarian stimulation: Personalized hormones (150–300 IU daily) to develop multiple follicles. Follicular monitoring: Ultrasounds and blood tests to determine the ideal retrieval time. Egg retrieval: Outpatient procedure with light anesthesia to collect mature oocytes. Vitrification: Rapid cooling and secure storage in liquid nitrogen. Benefits of vitrifying your eggs Control over your motherhood timeline. Preservation of egg quality against aging. Peace of mind when facing fertility-threatening treatments. Time to find the ideal partner without biological pressure. Emotional support throughout the journey At Ingenes, we combine cutting-edge technology with a personal approach. Our fertility psychologists provide personalized counseling and support sessions so you feel accompanied every step of the way. Technology that maximizes oocyte survival State-of-the-art equipment: High-precision vitrification to minimize cellular damage. Innovative protocols: Over 90% of eggs survive thawing. Continuous monitoring: High-resolution ultrasounds and constant serum measurements. For more details visit Egg vitrification: an option to preserve fertility or discover if freezing eggs at 40 is viable. Frequently asked questions 1. At what age is it most effective? The success rate is higher before age 35, when ovarian reserve and egg quality are optimal. Always consult a specialist and avoid self-medication. 2. How long do frozen eggs last? They can be stored indefinitely at –196 °C. At Ingenes, we periodically review samples to ensure viability. 3. What is the success probability? It depends on age and egg count. At Ingenes, we report >60% oocyte survival and a 45% pregnancy rate in women under 35. 4. Does retrieval hurt? It is performed under light sedation or intravenous anesthesia, so you won’t feel pain during the procedure. Discomfort lasts 24–48 hours, and our team provides the best post-operative care. Sources consulted American Society for Reproductive Medicine. (2020). Practice Committee Opinion: Mature oocyte cryopreservation. Fertility and Sterility, 114(1), 108–115. https://doi.org/10.1016/j.fertnstert.2020.03.012 National Cancer Institute. (2022). Cancer Terms: Egg Freezing. https://www.cancer.gov/publications/dictionaries/cancer-terms/def/egg-freezing MedlinePlus. (2021). Egg freezing. https://medlineplus.gov/eggsfreezing.html Practice Committee ASRM. (2013). Mature oocyte cryopreservation: A guideline. Fertility and Sterility, 99(1), 37–43. https://doi.org/10.1016/j.fertnstert.2012.09.025 We’re with you every step of the way. Don’t hesitate to seek guidance from a fertility specialist to make the best decision for your motherhood journey.