Don't miss our updates

The National Family Day is an opportunity to pause and recognize the richness of every family story in the United States. Today, families take many forms: from traditional to the most diverse, reflecting the openness and change of our society. What is National Family Day and why celebrate diversity? National Family Day is the day to honor every type of family: nuclear, single-parent, same-sex and more. It’s about celebrating inclusion, equality, and the unconditional love that binds every family, regardless of its structure. How has the American family evolved? According to Pew Research Center (2022), the nuclear family remains present, but other models have grown: Single-parent: rose from 12% in 1968 to 27% in 2014. Same-sex: over 1,000,000 same-sex couples living together in 2020 (Statista, 2021). Single parents by adoption or assisted reproduction, with IVF and egg donation. Single-parent families: challenges and strengths The increase is due to divorces, planned motherhood and assisted reproduction. Challenges include: Greater economic and time burden on a single caregiver. Need for support networks and attention to mental health. But these families also demonstrate great resilience and deep love. Impact of same-sex parenting With marriage equality and legal recognition, over 1,000,000 same-sex couples have formed families, contributing: Parenting based on empathy and conscious communication. Greater visibility and inclusion in public policies. Support on your path to parenthood At Ingenes we offer IVF, ICSI, egg and sperm donation with personalized protocols. Before self-medicating, consult a specialist in Assisted Reproduction to receive the guidance and follow-up your family deserves. We take every step with you, with empathy and expertise, because your dream of becoming a parent is unique and valuable. Celebrate family diversity all year round Events, resources and awareness campaigns keep family inclusion alive. For more ideas and actions, visit our article Celebrating family pride and diversity in June. Frequently Asked Questions (FAQ) What is assisted reproduction and how does it help different families? Techniques like IVF and ICSI assist couples with infertility, single mothers and same-sex couples, ensuring high-quality embryos. Always consult a medical specialist and avoid self-medication. What are the emotional challenges of a single-parent family? The responsibility of a single parent can generate stress and anxiety. Having support networks, help groups and therapy strengthens the emotional health of the whole family. How to promote inclusion of same-sex families at school? Equality policies, workshops and diverse materials raise awareness among educational staff. The participation of mothers and fathers in committees and collaboration with LGBTQ+ associations ensure safe environments. What resources support the mental health of first-time parents? The American Psychological Association and local groups offer guides and hotlines. A psychologist or family therapist can prevent burnout and strengthen the new dynamic. Sources Consulted Pew Research Center. (2022). Family Structures in America. Statista. (2021). Number of same‐sex couples in the United States. MedlinePlus. (2023). In Vitro Fertilization. American Society for Reproductive Medicine. (2022). Definition of infertility. Fertility and Sterility, 118(6), 1431–1442. Remember: every family is unique and every path to parenthood deserves professional attention. If you’re ready to take the next step, see a specialist in assisted fertilization and start your journey with the best support.
“Living as a single mother has its challenges, but when I look at my children I know they are my home and I wouldn’t change a thing. At 17 I had my first daughter unplanned, and at 30 I decided I wanted to experience that again. Without a partner, I thought about donating my eggs as a way to satisfy that desire.” “I looked into options and found the Institute. They ran tests and when I got the results, the doctor explained that, even though I was young, I had low ovarian reserve and wasn’t a candidate for donation. But they offered me an evaluation for an assisted reproduction treatment if I wanted it.” “I thought about it a lot and decided not to miss the opportunity. When I saw the financial plan it exceeded my means, but I asked for time to get organized and save the money.” How does egg donation pave the way for a second journey to motherhood? Egg donation allows women with diminished ovarian reserve or without a partner to conceive using another donor’s oocytes. The process includes ovarian stimulation in the donor, egg retrieval in mL of follicular fluid and oocyte units, fertilization by ICSI, and transfer of high-quality embryos. Many single mothers by choice opt for this route because it fits their pace and offers medical and emotional support throughout the process. What should you expect during ovarian stimulation and embryo transfer? Ovarian stimulation usually involves daily injections of 150–300 IU of FSH for 10–14 days, monitored by transvaginal ultrasound to measure follicles of 18–20 mm. Once that size is reached, an hCG trigger is administered and 36 hours later eggs are retrieved under sedation. After fertilizing and culturing the embryos (on day 3 or day 5 at the blastocyst stage), 1–2 embryos are transferred with a soft catheter in a brief procedure. How can emotional support influence assisted reproduction success? Stress and anxiety can raise cortisol and affect uterine receptivity. Integrating cognitive-behavioral therapy or mindfulness helps manage emotions, follow medical instructions, and reduce fear of failure. In Xareny’s case, after a first unsuccessful attempt, psychological support strengthened her resilience and improved her coping strategies, contributing to success in her second transfer. What financial planning tips should you consider? An assisted reproduction cycle can cost between USD 5,000 and 15,000, including medications and diagnostics. Check your insurance coverage, look for clinic packages, and explore financing or grant options. Saving EUR 200–300 per month in advance can ease the burden. Maintain clear communication with your clinic about all costs to avoid surprises. How does Xareny’s story inspire others? At 17, Xareny faced unexpected motherhood. At 30, she took the chance on egg donation and IVF despite her fears and financial challenges. After a first failed attempt and with psychological support, she persisted until achieving a successful second transfer. Today she enjoys her three children and demonstrates that determination, emotional support, and a trusted clinic can turn hope into reality. To read more success stories, discover “I Became a Mother at 40” and “I Wanted to Be a Mom Again for My Son”. Frequently Asked Questions 1. How long does an egg donation and IVF cycle take? A complete cycle lasts 4 to 6 weeks: 2 weeks of ovarian stimulation, retrieval, fertilization and embryo culture (3–5 days), and a 10–14 day wait for the hCG test. Timelines vary based on response and preliminary tests. Your specialist will provide a personalized schedule. 2. What are the success rates for donors with low ovarian reserve? Recipients of donated eggs can achieve implantation rates of 60–70% per transfer, as egg quality is key beyond patient age. Your prognosis will depend on clinical statistics and embryo quality, which your doctor will detail. 3. Are there medical risks associated with egg donation? Ovarian hyperstimulation syndrome (OHSS) is rare (

What are uterine fibroids and how can they impact fertility? Uterine fibroids are noncancerous growths in the muscle layer of the uterus. They can be as small as a pea or grow several centimeters wide, appearing inside the cavity, within the wall, or on the outer surface. Many women notice no symptoms, but some experience heavy periods, pelvic pressure, or discomfort. When fibroids change the shape of the uterine cavity or affect blood flow to the lining, they can make it harder for an embryo to implant and raise the chance of miscarriage. Why did it take me 10 years to conceive despite multiple treatments? “My husband and I married young—I was almost 20—and decided to wait before starting a family. When we tried to get pregnant naturally, nothing happened. An ultrasound showed ovarian cysts, so I started contraceptive pills as part of the treatment plan, and we scheduled our first insemination that November.” “I was 23 and hoped for success, but after six inseminations, we still had no baby. Every appointment ended in tears. I kept asking the doctors what was wrong, but I never got clear answers.” How did IVF with fibroids lead to success on the first transfer? Daniela, Ingenes mother, and her family “In 2016 we tried IVF at another clinic with two embryos, but it didn’t work. In 2019, we found this institute. They saw small fibroids on the outside of my uterus and reassured me they wouldn’t interfere. In September they transferred one embryo—and on the first try, it stuck. I cried tears of joy when the doctor called to say I was pregnant. After almost ten years of waiting, it finally happened.” What was my pregnancy and birth experience like after fibroids? Daniela and Angelina, Ingenes family “My pregnancy went smoothly. On May 17, 2020, my water broke early in the morning and by 7 a.m., our daughter Angelina was born. It was so fast! When they placed her in my arms, I felt like I was dreaming—tiny fingers, tiny toes. My husband was by my side, talking and kissing my belly all through pregnancy. That pure love carried us through every moment.” “All those years of frustration melted away the moment we met her. She completed our family.” What should you know before starting fertility treatment with fibroids? Never self-medicate. If you’re thinking about fertility treatments, talk to a reproductive specialist first. Fibroid size, position, and type vary greatly, and only a personalized assessment can determine the best plan for you. To read more success stories, visit “I had uterine fibroids and became a mother with IVF” or “I have endometriosis and got pregnant after 10 years”. FAQ 1. Can small fibroids outside the uterus really not affect IVF success? Yes. Subserosal fibroids—those on the outer uterine wall—usually don’t change the shape of the cavity or interfere with implantation if they’re under 3 cm and asymptomatic. Specialists use ultrasound or MRI to check size and location. Always discuss your individual case to decide if surgery is needed or if you can go straight to IVF. 2. What are common treatments for fibroids when trying to conceive? Treatment depends on fibroid type, size, symptoms, and your fertility goals. Medical options include short-term GnRH agonists or antagonists to shrink fibroids, with possible side effects like hot flashes. Surgically, myomectomy can be done by hysteroscopy (for inside-cavity fibroids), laparoscopy (small outer fibroids), or open surgery (large or multiple fibroids). Recovery before trying pregnancy ranges from 1 to 6 months, depending on the approach. 3. How does the IVF protocol change for women with fibroids? Ovarian stimulation is similar—gonadotropins to grow around 10–20 follicles with estradiol (E2) monitors in pg/mL. The main adaptation is ensuring the transfer catheter navigates any contour changes in the uterus, often using ultrasound guidance. Many women with small, non-distorting fibroids proceed with a standard protocol and achieve great results. 4. What follow-up care is recommended after giving birth post-IVF with fibroids? After delivery, track your menstrual cycle and fibroid growth with regular exams and pelvic ultrasounds every 6–12 months. If heavy bleeding (>80 mL per cycle) or pain returns, discuss medical or surgical options. Maintaining a healthy weight (BMI 18.5–24.9), a fiber-rich diet, regular exercise, and supplements like vitamin D and omega-3s may help slow fibroid growth. References American College of Obstetricians and Gynecologists. (2021). Uterine Fibroids. https://www.acog.org MedlinePlus. (2022). Uterine Fibroids. https://medlineplus.gov/uterinefibroids.html Pritts, E. A., Parker, W. H., & Olive, D. (2020). Fibroids and infertility: an update. Obstet Gynecol, 135(4), 28S–34S. doi:10.1097/AOG.0000000000003722 Somigliana, E., Vercellini, P., Parazzini, F., et al. (2019). Fibroids and ART outcomes: systematic review. Hum Reprod Update, 25(1), 130–142. doi:10.1093/humupd/dmy035 Stay hopeful: every journey is unique. If you’re facing fibroids and fertility challenges, reach out to a specialist in assisted reproduction. You don’t have to go through this alone.

In Oregon, United States, Philip and Rachel Ridgeway have just welcomed their twins conceived more than thirty years ago, thanks to embryos frozen in 1992 and donated by the National Embryo Donation Center in Knoxville, Tennessee. Philip Ridgeway and Rachel Ridgeway What is cryopreservation and how does it protect embryos? Cryopreservation involves freezing embryos at –196 °C (liquid nitrogen) to keep them viable until transfer, usually at the blastocyst stage (day 5–6 after fertilization). The process begins like IVF: ovarian stimulation, egg retrieval, fertilization, and then ultra-rapid freezing at –320 °F. Embryos cryopreserved at subzero temperatures How were twins born from embryos frozen for 30 years? Dr. Karla Yasmín Santiago, a Reproductive Biology specialist, notes that early cryopreservation techniques were less precise, making this case extraordinary. Today, 80 % of embryos survive thawing, but without rigorous lab monitoring pregnancy rates rarely exceed 50 %. “This result is impressive: early methods lacked today’s precision. Even now, only about 80 % of embryos survive thawing and fewer than 50 % achieve pregnancy without strict control and good maternal health.” Dr. Santiago Embryologist at the Ingenes Institute, Mexico City The Spanish Fertility Society (SEF) reports that 80 % of blastocysts survive thawing and pregnancy rates range from 20 % to 50 %. MedlinePlus reports similar figures. How has cryopreservation improved today? With vitrification and advanced protocols, survival exceeds 90 % and pregnancy rates increase. Modern incubators precisely control gases (O₂, CO₂) and temperature. Genetic testing (PGT-A) helps select embryos with the highest chance of a healthy baby. “Today you can freeze your embryos for as long as you need, whether for medical or personal reasons. However, personalized diagnostics are key to success.” Dr. Santiago How to preserve my fertility with cryopreservation? If you’re considering fertility preservation, learn about our preservation services and start with a comprehensive reproductive health assessment. At Ingenes we guide you on freezing eggs or embryos. Schedule your appointment to design a personalized plan and increase your chances of pregnancy. Don’t self-medicate: always consult a Reproductive Medicine specialist. Frequently Asked Questions 1. How Long Can Frozen Embryos Remain Viable? Properly vitrified embryos can remain viable indefinitely. There are successful births after more than 25 years of storage. Key factors are ultra-rapid cooling rates and stable storage at –196 °C, with constant monitoring to prevent crystal formation. Since the 1990s, protocols have improved post-thaw survival to over 90 %, though initial embryo quality and lab expertise remain critical. 2. What Factors Influence Survival After Thawing? Survival depends on embryo quality, vitrification solution composition, cooling and warming rates, and storage stability. Blastocysts (day 5–6) generally withstand thawing better. Lab conditions such as low O₂ levels (5 %), stable temperature, and high-purity nitrogen reduce oxidative stress. The embryologist’s skill is essential for precise thawing. 3. Are There Risks in Transferring Frozen Embryos? Risks are similar to traditional IVF: multiple gestations, ovarian hyperstimulation syndrome (in fresh cycles), and ectopic pregnancy (

Jennifer Aniston, 53, said: “I would have given anything if someone had told me, ‘Freeze your eggs. Do yourself a favor’. You never think about it until time passes and the ship sails.” “In my late 30s and into my 40s, I went through very tough times. I was trying to get pregnant. It was a complicated journey on the path to starting a family.” After years of speculation about her motherhood, the actress revealed: “I underwent In Vitro Fertilization, I took Chinese infusions, I tried everything.” What does “freeze your eggs” mean? When Jennifer says “Do yourself a favor. Freeze your eggs”, she encourages preserving future fertility through vitrification of mature oocytes, which are stored at –196 °C in liquid nitrogen to halt biological aging. Elective cryopreservation is a strategic option to keep reproductive potential active until personal, professional, or health circumstances are right. As explained in this article, it’s a key decision for your family’s future. Step-by-step process Ovarian stimulation: Daily injections of FSH and LH for 10–12 days to develop multiple follicles. Trigger injection: 10,000 IU of hCG or a GnRH agonist for final maturation. Egg retrieval: Ultrasound-guided follicular aspiration under light sedation. Vitrification: Ultra-rapid freezing in cryoprotectant solutions without forming ice crystals. Storage: Preservation at –196 °C in liquid nitrogen, even for decades. Quality report: Assessment of the number, maturity, and morphology of the oocytes. Who should consider it? Women diagnosed with cancer before chemotherapy or radiotherapy. Those with endometriosis or low ovarian reserve. Women under 35 focused on career but wishing to delay motherhood. Anyone with conditions that may affect ovarian function. Deciding when to become a mother is very personal. Egg freezing offers autonomy and relieves biological clock pressure. For those over 40, it can still be an option, though success rates decline with age. Benefits and risks Benefits: Preserves fertility before ovarian aging or gonadotoxic treatments. Reduces anxiety about the biological clock. Provides flexibility in family planning. Mild risks: ovarian hyperstimulation syndrome, anesthetic complications <1%, emotional stress. Consulting a specialist is key to tailor the protocol and manage expectations. Frequently asked questions 1. How many eggs should I freeze to improve my chances? It depends on your age and ovarian reserve. Under 35, women typically aim for 15–20 eggs to achieve a 50–60% live birth rate. Over 38, 20–30 eggs may be needed due to lower survival and fertilization rates after thawing. 2. Does it guarantee a future pregnancy? It doesn’t guarantee, but it increases the odds. Egg quality, tied to age, is crucial. Studies show 90% survival post-vitrification and 35–40% implantation per transfer. 3. Can I use my eggs at any age? Legally, up to 50–55 years. Biologically, maternal health matters. Your specialist and obstetrician will assess your condition before transfer. 4. How long can I store my eggs? Indefinitely, with successful births after more than 10 years. Consent is renewed every 5 years per regulations, and temperatures are monitored to maintain integrity. References American Society for Reproductive Medicine. (2022). Practice Committee Opinion: Oocyte cryopreservation. Fertility and Sterility. MedlinePlus. (2023). Egg Freezing. U.S. National Library of Medicine. Practice Committee ASRM. (2013). Mature oocyte cryopreservation: guideline. Fertility and Sterility. ESHRE. (2021). Guideline on female fertility preservation. Human Reproduction Open. We know this journey can feel overwhelming. Every story is unique and deserves personalized attention. We invite you to contact an assisted reproduction specialist to answer your questions and design a tailored plan. We are with you every step of the way.

Los riesgos de tener un bebé a los 40 no deben detenerte. Inés te cuenta su historia, sus miedos y cómo logró a sus 2 pequeñas a los 46 con FIV.
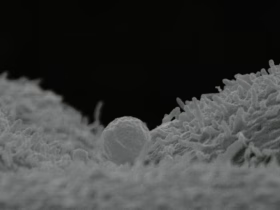
A mother carrying a baby in her womb alters its genes, even when the egg comes from another woman. This means her child will be born with traits similar to hers, according to a study by the Valencia Infertility Institute Foundation (IVI). How does the maternal uterus influence the genes of a donated embryo? The uterus is much more than a container: during gestation there is constant dialogue between embryo and endometrium. Endometrial fluid exosomes release maternal RNA that reaches the embryonic nucleus and regulates gene expression, adjusting physical and health traits. Studies such as “The Marvelous Science of Egg Donation: Beyond Genes” explain this in detail. Electron microscope of an exosome about to adhere to the endometrium (IVI). For nine months, the embryo receives blood, nutrients, and oxygen through the umbilical cord. These biochemical signals vary according to the gestational carrier’s genetics, habits, and lifestyle, reinforcing that egg donation is only the starting point. It is the uterus that shapes and “signs” the DNA that will guide the baby’s development. What epigenetic changes can gestation cause in egg donation? During gestation, epigenetic interaction can influence: Eye color and shape Hair texture and tone Facial expressions, such as the smile Predisposition to certain metabolic or autoimmune diseases These modifications do not replace the donated genetics but regulate the activation or silencing of specific genes. To learn more, see “The Revolutionary World of Fertility and Egg Donation”. How does genetic exchange occur between embryo and endometrium? Exosome releasing maternal RNA into the cytoplasm of a blastocyst (IVI). Exosomes, 50–150 nm vesicles, transport maternal RNA to the blastocyst’s cytoplasm and adjust gene transcription. The result is a unique epigenetic profile that combines the donor’s inheritance and the carrier’s influence. Why is egg donation a great opportunity? Rocío, 52, had her two babies via egg donation at Ingenes. The egg donation experience lets you carry and give birth to a child with a unique maternal genetic imprint. Avoid self-medication and always consult a Assisted Reproduction specialist before starting any fertility treatment. Frequently Asked Questions about egg donation and uterine genetics 1. Does the gestational mother contribute DNA if the eggs are from another person? Yes. Although the main genetic load comes from the donor, during gestation the uterus releases exosomes with RNA that modulate the embryo’s gene expression, influencing physical traits and future health. 2. What risks or benefits does this genetic interaction have? Benefits include better embryo adaptation to the uterine environment and higher implantation rates. As for risks, long-term impact is still under study: so far there is no evidence of adverse effects, but specialized prenatal follow-up is recommended. 3. Can it influence the baby’s temperament? Personality arises from genetics and environment. Egg donation and uterine influence affect physical traits and biochemical predispositions, but parenting style and the postnatal environment are key to the child’s character. 4. How to choose the best clinic for egg donation? Choose centers with international accreditations, multidisciplinary teams, and evidence-based protocols. Review their success rates, lab technology, and psychological support offered before and after birth. Sources Vilella F. et al. (2015). Hsa-miR-30d, secreted by the human endometrium, is taken up by the pre-implantation embryo and might modify its transcriptome. Development, 142(18), 3210–3221. MedlinePlus. (2023). Assisted Reproductive Technology. U.S. National Library of Medicine. Gardiner K. et al. (2020). Epigenetic modifications during pregnancy: maternal-fetal interactions. Journal of Reproductive Immunology, 138, 103-110. Mor & Cardenas. (2018). The immune system in pregnancy: a unique complexity. American Journal of Reproductive Immunology, 79(3), e12847. We are with you on this journey. If you have questions or are considering egg donation, consult an Assisted Reproduction specialist for the best guidance and support.

Con un tratamiento de Reproducción Asistida multiciclo, Marisol y su esposo lograron tener a sus cuatitos en su tercer ciclo de Fertilización In Vitro.

On November 4, the documentary “My Mind & Me” by Selena Gomez premiered, where she shares key moments of her life, focusing on her mental health and some of the physical conditions she faces. Selena Gomez and her dream of becoming a mother: challenges with bipolar medication Selena confessed that one of her greatest desires is to become a mother. However, some treatments for bipolar disorder can increase the risk of neural tube defects, cardiac or neurobehavioral issues in the fetus, making a natural and healthy pregnancy more complex. Assisted reproduction options for those on psychiatric medication Thanks to advances in assisted reproduction, it is possible to plan a pregnancy safely. In vitro fertilization (IVF) with preimplantation genetic testing (PGT) allows the selection of embryos without anomalies. And if a direct pregnancy poses a high risk, surrogacy is a solution: another woman carries the baby and, once born, the intended parents receive it. How the Ingenes Initial Program helps At Ingenes we design tailored plans, adjusting medication doses, recommending healthy lifestyle habits, and providing close monitoring. We use evidence-based protocols (for example, 150–300 IU/day of FSH and embryo culture in 5–6 mL of medium) along with continuous emotional support. Do not self-medicate: always consult a reproductive specialist before starting any treatment. Many women, like Selena, have had successful pregnancies under our care. Schedule an appointment and discover your ideal path to motherhood. Frequently Asked Questions 1. Why do bipolar disorder medications affect fertility? They can alter hormonal function, interfere with ovulation, and increase the risk of malformations. A specialist can adjust doses, propose cryopreservation, or recommend IVF with PGT to reduce risks. 2. Can I become pregnant if I have bipolar disorder? Yes. With planning—coordination between a psychiatrist and fertility expert, medication adjustments, hormone monitoring (LH, FSH), and frequent ultrasounds—a pregnancy can be safe for you and your baby. 3. When is surrogacy useful? When the risks to the mother are very high. An altruistic gestational carrier carries the pregnancy, using protocols like the transfer of 1–2 embryos (quality ≥ BB) with estrogens (6 mg/day) and progesterone (600 mg/day) for optimal implantation. 4. What results does the Ingenes Initial Program offer? We combine diagnosis, serial ultrasounds, and hormonal adjustments (FSH, LH) to achieve pregnancy rates ≥ 60% in women under 35 and ≥ 50% in women over 35. Our comprehensive approach includes constant emotional and nutritional support. Sources ACOG. Practice Bulletin No. 214. Obstetrics & Gynecology, 138(2), e1–e20 (2021). MedlinePlus. Bipolar Disorder and Pregnancy. U.S. National Library of Medicine (2022). Royal College of Psychiatrists. Bipolar disorder: management during pregnancy and postpartum. Br J Psychiatry, 217(1), 25–32 (2020). SART. Fertility Clinic Success Rates (2021). Remember: every case is unique. Keep hope alive and always seek the guidance of an assisted reproduction specialist to accompany you on this journey.
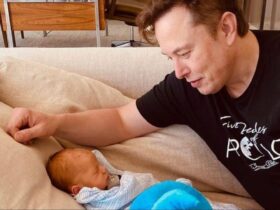
Elon Musk considera que la humanidad se dirige a su fin inminente, a menos de que las personas en todo el mundo comiencen a tener más hijos.

We know that as maternal age increases, the probability of the baby having a genetic anomaly also rises. The following chart shows the estimated risk of Down syndrome by the mother’s age: What is Clarix and what is it for? Clarix is a noninvasive prenatal genetic test that analyzes your baby’s health and tells you its sex from week 10 of pregnancy. It works the same whether your pregnancy was natural or via assisted reproduction. At Ingenes we perform this test with no risk to you or your baby. With just 10 mL of your blood, we obtain cell-free fetal DNA and achieve 99% accuracy. How does the Clarix test work step by step? We draw 10 mL of maternal peripheral blood. We isolate and sequence the cell-free fetal DNA. We detect the most common aneuploidies (trisomy 21, 18, and 13). We provide you with a report showing results and 99% accuracy. Who is Clarix recommended for and when to take it? Learn Marisol’s story, who got pregnant despite PCOS. Clarix is ideal for: Pregnant women (natural or after assisted reproduction). Those aged 35 or older with higher risk of chromosomal anomalies. Those who want to know fetal sex from week 10. Patients who did not undergo PGT-A during their treatment. In what formats is the Clarix test offered? Contact us and we will create your personalized plan so you feel confident about your baby’s health. Also learn about PGT-A for extra peace of mind. Importance of early genetic diagnosis Detecting anomalies noninvasively gives you information to make calm decisions, reduces anxiety, and allows proper follow-up. You avoid risks associated with invasive tests like amniocentesis. With Clarix you receive fast, accurate results to plan everything with your doctor. Do not self-medicate without consulting a specialist first. FAQ about Clarix and genetic anomaly detection 1. Is Clarix safe for me and my baby? Yes. It is 100% noninvasive: only a 10 mL maternal blood sample is required, with no risk of miscarriage or complications. Massively parallel sequencing provides 99% accuracy for trisomies. 2. What anomalies does Clarix detect? It detects trisomies 21 (Down), 18 (Edwards), and 13 (Patau). Depending on the format, it may include sex chromosome anomalies or microdeletions. For a more comprehensive analysis, consider PGT-A. 3. When do I get the results and how? Within 5–7 business days you will receive a detailed report by email and can schedule a consultation with our maternal-fetal medicine specialists to answer questions and plan follow-up. 4. Do I need fasting or special preparation? No fasting or special preparation is required. You only need to provide a 10 mL blood sample at our lab or affiliate center. If you have allergies or medical conditions, mention them beforehand to ensure your comfort. References American College of Obstetricians and Gynecologists. (2022). Noninvasive Prenatal Testing. Retrieved from https://www.acog.org MedlinePlus. (2023). Genetic Testing and Pregnancy. https://medlineplus.gov/genetictestingandpregnancy.html Lo, Y. M., & Chiu, R. W. (2017). Cell-free DNA sequencing in maternal plasma for prenatal diagnosis. Clinical Chemistry, 63(1), 49–58. doi:10.1373/clinchem.2016.260226 Gregg, A. R., et al. (2016). Fetal Aneuploidy Detection: ACOG Practice Bulletin. Obstetrics & Gynecology, 127(5), e123–e137. doi:10.1097/AOG.0000000000001610 We’re with you on this journey: if you have questions or concerns, always consult an assisted reproduction specialist for proper guidance and support.

El esperma para la inseminación artificial debe ser de un donante o pareja, nunca del especialista. Descubre por qué en Ingenes no sucedería esto.

Every April 25 we celebrate DNA Day, a date that recognizes one of the greatest discoveries of the 20th century: the double helix structure of DNA. Since Watson and Crick described it in 1953, DNA has changed our view of life, inheritance, diseases and, above all, reproductive and genetic medicine. In this article we explore why DNA is fundamental, how it has driven medical treatments—especially in fertility and assisted reproduction—and why it will continue to be the cornerstone of future medicine. To get a closer look at the day-to-day life of a geneticist, visit Today Is a Geneticist’s Day. What is dna and why do we celebrate it? DNA (deoxyribonucleic acid) is the molecule that stores the genetic information of all living beings. It resides in the nucleus of every cell and passes hereditary traits from generation to generation. Celebrating April 25 marks the 1953 Nature publication that revealed the double helix and paved the way for genetic engineering, molecular diagnostics, gene therapy and personalized medicine. How does the double helix function as the language of life? The double helix consists of two twisted strands with four nitrogenous bases: adenine (A), thymine (T), cytosine (C) and guanine (G). A pairs with T and C with G, forming a unique code in each person (except identical twins). That code dictates how cells function, reproduce and survive. How has dna transformed modern medicine? Understanding DNA enabled the development of genetic tests for: Paternity and kinship testing Diagnosis of rare genetic disorders Compatibility studies for organ donation Detection of hereditary risks for breast cancer, colon cancer or cardiovascular diseases Personalized treatments based on genetic profile These advances have revolutionized diagnosis and therapy across all specialties. What role does dna play in fertility and assisted reproduction? Genetic testing is key in fertility clinics, as it increases the chances of a healthy pregnancy. The main procedures include: Genetic Preimplantation Testing in IVF PGT-A and PGT-M: During in vitro fertilization, embryos are analyzed with PGT-A (aneuploidy detection) and PGT-M (monogenic disorders such as cystic fibrosis or muscular dystrophy). This way we select the healthiest embryos and avoid hereditary conditions. Genetic Compatibility Testing for Couples Compatibility test: Detects recessive mutations that could combine and affect the baby. It’s essential in egg or sperm donation and guides decision-making. Genetic fertility assessment: Identifies genes that influence spermatogenesis or ovarian function, explaining hidden causes of infertility. Can DNA solve unexplained fertility problems? Yes. A comprehensive genetic analysis clarifies: Recurrent miscarriages due to chromosomal abnormalities in the embryo. Low sperm count caused by microdeletions on the Y chromosome. Prevention of hereditary diseases through IVF with PGT-M. What does the future hold for DNA in reproduction? Genomic sequencing paves the way for AI-driven genetic analyses, gene therapies for infertility mutations, ultra-precise genomic profiling and ethical gene editing. At Ingenes we have our own laboratory and experts in genetics, embryology, reproductive medicine and counseling. Discover our vision at Celebrating Hope and Science. Frequently Asked Questions about DNA and Reproductive Genetics How Does DNA Day Drive Advances in Assisted Reproduction? This day reminds us of the power of genetics to improve embryo selection, reduce pregnancy losses and prevent hereditary diseases. Every year, we celebrate how DNA knowledge optimizes outcomes and hope. Avoid self-medication and, before any genetic test, consult an assisted reproduction specialist. What Safety Measures Are in Place for Genetic Testing in IVF? PGT-A and PGT-M follow strict controls: sterile sample handling, validated protocols on calibrated equipment and ethical committees ensuring reliability and safety. Specialists interpret results alongside embryo morphology to maximize success rates and minimize risks. Always consult an expert before any procedure. Can Genetics Predict All Fertility Problems? Genetic tests detect many hereditary causes—chromosomal abnormalities and specific mutations—but don’t explain factors like age, hormonal imbalances or uterine anatomy. That’s why combining genetic analysis with hormonal studies and imaging is key. Your specialist will recommend the appropriate protocol. How to Prepare Emotionally and Medically for Genetic Testing? Emotionally, counseling helps you cope with results, discuss ethical concerns and set realistic expectations. Medically, blood tests (hormones in mIU/mL), imaging studies and lifestyle adjustments are required. All decisions are made together with your partner and medical team. Empathetic communication and psychological support make the difference. Sources Consulted National Library of Medicine. (2023). DNA Structure. MedlinePlus. https://medlineplus.gov/genetics/understanding/dna International Society for Prenatal Diagnosis. (2022). Guidelines for PGT-A & PGT-M. doi.org/10.1002/pd.6123 American Society for Reproductive Medicine. (2021). Genetic Causes of Male Infertility. doi.org/10.1016/j.fertnstert.2021.01.012 Nature Editorial. (1953). Molecular Structure of Nucleic Acids. Nature, 171(4356), 737–738. doi.org/10.1038/171737a0 We accompany you on this journey: each step brings you closer to your dream of becoming a mother or father. If you have any questions, always consult a fertilization specialist.

Noemí decidió que su deseo de ser madre soltera era más grande que cualquier prejuicio. Conoce su historia y cómo tuvo a sus cuatitas a los 46.

On February 28, 2022, Ingenes opened its doors in Cancún to support your desire to build a family with assisted reproduction and advanced genetic services in the Mexican Caribbean. Since then, Ingenes Cancún has established itself thanks to its team of highly trained doctors and specialists, modern facilities, and state-of-the-art technology. Ingenes Cancún team What makes Ingenes Cancún a leader in assisted reproduction? Under the direction of Dr. Israel Rodríguez Trejo, we combine continuous education, cutting-edge technology, and a personal approach. “For me, the institute has been an inspiration seeing patients become pregnant and welcome their babies.” “We don’t see patients as numbers. We get to know each one, their story, and the dream they want to achieve.” Dr. Israel Rodríguez Trejo Dr. Israel with a couple of little ones he helped bring into the world How does Ingenes Cancún support international patients? We receive patients from Switzerland, Canada, the U.S., Brazil, Guatemala, Spain, and Peru. We offer comprehensive IVF protocols, genetic analyses, and emotional support. Medical tourism in Cancún eases your journey; we handle personalized care from day one. “We hold continuous improvement sessions to align efforts toward the same goal: ensuring every patient has a warm experience and realizes their dream.” Dr. Israel Rodríguez Trejo For surrogacy, explore Surrogacy in Mexico: Building Families with Ingenes Expertise. If you prefer the northern border, visit Ingenes Mexicali: Making Dreams Come True on the Southern Border. Personalized team care Workshops, team-building activities, and open communication ensure every embryologist, nurse, and specialist understands your needs and provides empathetic support. Do not self-medicate without consulting a specialist. Why choose Ingenes Cancún? Our innovation, empathy, and safety, along with success rates supported by peer-reviewed studies, make us a reference in reproductive medicine. If you want to increase your chances of pregnancy, first consult a specialist in assisted reproduction. Frequently Asked Questions 1. What treatments does Ingenes Cancún offer? In vitro fertilization (IVF), artificial insemination, PGT-A, egg donation, and surrogacy. Everything is tailored to your medical history and emotional state. The process includes a comprehensive evaluation, ovarian stimulation (150–225 IU of FSH/day), and embryo transfer in a 25 mL culture medium. 2. How do I prepare my trip as an international patient? Choose daily flights to Cancún, arrange a medical visa, and book accommodation near the clinic. We advise you on lodging, transfers, and translation. Upon arrival, you’ll receive your treatment plan in your language: ultrasounds, blood tests, and psychological support, all coordinated to reduce your stress. 3. What are the costs of an IVF cycle? A basic cycle with ICSI ranges from USD 4,500 to USD 6,500; egg donation adds USD 3,000–3,500; PGT-A adds USD 800–1,200. Includes consultations, ultrasound monitoring, punctures (5–10 mL per follicle), and embryo culture to the blastocyst stage. 4. How do I manage the emotional aspect? We include reproductive psychology with four 1-hour sessions to reduce anxiety, support decision-making, and offer support groups. Emotional well-being improves implantation and prevents dropout. We have specialized therapists and relaxation activities. Sources American Society for Reproductive Medicine. (2021). Guidelines on terminology for assisted reproductive technologies. Fertility and Sterility. MedlinePlus. (2022). In Vitro Fertilization. U.S. National Library of Medicine. Practice Committee ASRM. (2020). Diagnostic evaluation of the infertile female: a committee opinion. Fertility and Sterility. World Health Organization. (2019). Infertility definitions and terminology. WHO. We know this journey can be challenging. We are here to support you with professionalism and warmth. Consulting a specialist in assisted reproduction is the best first step to fulfilling your dream of becoming a parent.

“`html What is hyperthyroidism and how does it affect fertility? The thyroid gland sits just below the “Adam’s apple” and looks like a butterfly. It makes two main hormones, T4 (thyroxine) and T3 (triiodothyronine). When it goes into overdrive and pumps out too much of these hormones, we call that hyperthyroidism. Anyone can get it, but women are eight times more likely than men. Too many thyroid hormones speed up your metabolism and throw your menstrual cycle off balance. You might get irregular periods, long stretches without any bleeding, very heavy flow or cycles where no egg is released. All of these changes make it harder to conceive naturally. If you’re planning a pregnancy, getting your thyroid in check is key. How does hyperthyroidism alter menstrual cycles and ovulation? High T3 and T4 levels upset the delicate communication between your brain and ovaries, and you may notice: Irregular or missed periods Very heavy or prolonged bleeding Cycles without ovulation These shifts can make getting pregnant tougher. If you think your thyroid might be the culprit, don’t self-medicate. Talk to a doctor and book an appointment with a fertility specialist. What are the common symptoms of hyperthyroidism? When your thyroid goes into overdrive, you might experience: Losing weight even if your appetite is normal Feeling anxious or irritable Fast heartbeat and feeling overheated Excessive sweating Frequent bowel movements Higher risk of bone thinning Brittle hair and nails What causes hyperthyroidism and who is at risk? The main cause is Graves’ disease, an autoimmune condition where your body’s antibodies push the thyroid to make too much hormone. Other triggers include: Too much iodine in your diet Thyroid nodules or cysts Thyroid inflammation (thyroiditis) Noncancerous pituitary tumors How is hyperthyroidism diagnosed before pregnancy? An endocrinologist will examine your thyroid size, check your pulse, skin and eyes, then run blood tests. A low TSH (0.5–3.5 mU/mL) alongside high T3 and T4 confirms hyperthyroidism. Early diagnosis helps restore balance and protect your fertility. What treatment options are safe if you want to conceive? The goal is to bring your thyroid hormones back to normal under medical care. Treatments include: Anti-thyroid pills to lower T3 and T4 Radioactive iodine therapy in specific cases Once your hormones are steady, ovulation often resumes and fertility improves. You’ll still need careful monitoring during pregnancy. If medication alone doesn’t do the job, IVF might be recommended. At Ingenes, our IVF process—ovarian stimulation, egg retrieval, fertilization and embryo transfer—is customized to give you the best chance. For more in-depth information, see our pages on Hypothyroidism and fertility and Hypothyroidism and Fertility: What You Need to Know. FAQ Can hyperthyroidism treatment improve my chances of pregnancy? Yes. Correcting your thyroid levels with medication or iodine restores your cycle and ovulation. Most women see results within a few months. Stay in touch with your endocrinologist and fertility specialist to adjust treatment safely. Leaving hyperthyroidism untreated can increase miscarriage risk or lead to early labor. Managing it before trying to conceive gives you and your future baby a healthier start. Is it safe to use radioactive iodine if I want to conceive soon? Radioactive iodine works well but means waiting 6–12 months before trying to get pregnant so your body clears the radiation. Use reliable birth control during this time. After that, you can try under your doctor’s guidance. If you’re on a tighter timeline, anti-thyroid drugs might be a better choice. Discuss your options with your specialist to find what fits your plans and goals. How do I differentiate between hyperthyroidism and other causes of irregular cycles? Stress, weight shifts or PCOS can disrupt periods, but hyperthyroidism often brings whole-body symptoms—weight loss, overheating, fast heartbeat. A simple blood test measuring TSH, T3 and T4 gives a clear answer. Tell your doctor about all your symptoms and ask for thyroid tests if you notice a pattern. Early detection helps avoid complications during fertility treatment. What should I avoid if I have hyperthyroidism? Skip high-iodine foods—excess seafood, iodized salt or supplements—unless your doctor approves. Also, don’t try herbal “thyroid boosters” on your own. Always check with a fertility specialist before adding any remedy. Stick to a balanced diet, stay hydrated and follow your treatment plan. Regular check-ups make sure your hormones stay in the sweet spot for conception and a healthy pregnancy. Sources MedlinePlus. (2023). Hyperthyroidism. Retrieved from https://medlineplus.gov/hyperthyroidism.html American Thyroid Association. (2022). Hyperthyroidism. doi:10.1089/thy.2021.0178 Jameson, J. L., & Mandel, S. J. (2021). Harrison’s Endocrinology (4th ed.). McGraw-Hill Education. Stagnaro-Green, A., et al. (2019). Thyroid and pregnancy: An updated review. Journal of Clinical Endocrinology & Metabolism, 104(12), 5607–5615. doi:10.1210/clinem/dgz147 We’re here with you on this journey. Don’t lose hope—getting your thyroid under control is the first step toward starting your family. Talk to a fertility specialist to build a personalized plan and move confidently toward parenthood. “`

When you think about fertility and the magical wait for a baby, technology becomes a fundamental ally. Kourtney Kardashian shared how an ultrasound saved her future little one’s life during her fertility journey. At Ingenes, we know how valuable this resource is and how it can make a difference on your path to motherhood or fatherhood. What is an ultrasound and how does it impact fertility? An ultrasound is a non-invasive imaging technique that uses high-frequency sound waves to show the baby’s development in real time. It allows you to: Monitor fetal growth. Measure amniotic fluid in mL. Detect complications like ectopic pregnancies early. And, of course, strengthen that emotional bond by providing your baby’s first image. How do cutting-edge technologies improve IVF success? From controlled ovarian stimulation to embryo transfer, advances in imaging and lab work are key. At Ingenes, we use 3D and Doppler ultrasound to measure follicles in mm and uterine blood flow, fine-tuning hormonal protocols. This high-resolution monitoring increases implantation rates and promotes healthier pregnancies. Why is ultrasound essential in IVF and reproductive health? Each stage of IVF is guided by ultrasound: Verifying follicle count and size before egg retrieval. Checking endometrial thickness in mm to optimize transfer. Confirming implantation after the procedure. Our specialists interpret these images and make informed decisions to boost your chances of success. Personalized care and technology hand in hand At Ingenes, we combine empathy and expertise. Beyond technology, we build your medical history and offer emotional support. We tailor each protocol—medications in µg or IU—to your unique profile. Avoid self-medicating. You’ll meet our Assisted Reproduction specialists to discuss your goals and questions. If you want to learn how Artificial Intelligence is transforming treatments or discover new innovations beyond age limits, we’ll be here to support you. Preparation for your first fertility ultrasound Before your ultrasound: You may need a full bladder for pelvic images. Do not apply lotions on your abdomen. Bring all your questions to an Assisted Reproduction specialist. Frequently Asked Questions Can ultrasounds detect all fertility problems? They help visualize ovarian cysts, fibroids, assess endometrial thickness, and count antral follicles in PCOS. They do not measure genetic or hormonal imbalances: that’s where blood tests (FSH, LH, AMH) and genetic studies come in. How often should I have ultrasounds during IVF? During stimulation, they are usually every 2–3 days to track growth until 18–20 mm. Then the trigger injection is given; egg retrieval occurs 36 hours later. An ultrasound at 6–7 weeks confirms implantation. Are there risks associated with ultrasound? It’s safe in professional hands. It uses non-ionizing waves and follows the ALARA principle to ensure the lowest possible exposure. How can I prepare emotionally? Join support groups, practice yoga or meditation, and talk with your partner and medical team. At Ingenes, we offer counseling to help you build resilience. Sources Consulted American College of Obstetricians and Gynecologists. Practice Bulletin No. 211 (2022). National Library of Medicine. Antral Follicle Count. MedlinePlus (2023). Practice Committee of the ASRM. Diagnostic evaluation of the infertile female (2021). World Health Organization. Laboratory manual for semen (6th ed., 2021). Remember: each ultrasound brings you one step closer to your dream. Count on our support and, if you have any questions, consult a fertilization specialist for the best guidance and accompaniment.

“`html What is oocyte quality and why does it matter for your fertility? As years go by, especially after age 35, not only does the number of eggs in the ovaries decrease, but their quality does too. Oocyte quality reflects an egg’s ability to develop into a healthy embryo after fertilization. How do you know if your eggs are high quality? A high-quality egg has the correct number of chromosomes and the energy needed to grow and divide properly. If quality is low, the risk of chromosomal abnormalities and reproductive failure increases. Hormones like FSH and estradiol are measured to assess ovarian response. But the most accurate evaluation comes with an in vitro fertilization cycle and preimplantation genetic testing. Factors that can affect oocyte quality Besides age, there are other factors that can influence even young women: Genetic or immunological disorders Cancer treatments Tobacco use Endometriosis Obesity Polycystic ovary syndrome Options if oocyte quality is low There is no treatment that directly improves egg quality, but in vitro fertilization increases the chances of success. When your own eggs aren’t viable, egg donation is a highly effective option. At Ingenes, we combine cutting-edge technology with personalized care. We analyze the 10 causes of poor oocyte quality and support you emotionally throughout the process to give you confidence every step of the way. Ovarian reserve: what it is and how it’s measured Ovarian reserve is determined by the anti-Müllerian hormone (AMH) and the antral follicle count (AFC) via ultrasound. These values predict how many eggs you might retrieve and their potential quality. Knowing your reserve helps plan the best path to fulfill your desire to become a parent. How Ingenes supports you At Ingenes we offer: A team of assisted reproduction specialists Ongoing emotional support Protocols with preimplantation genetic testing Blastocyst-stage embryo transfer Remember: avoid self-medication. To protect your fertility, the best step is to see an assisted reproduction specialist. Frequently Asked Questions Can I Improve My Egg Quality with Lifestyle Changes? Eating an antioxidant-rich diet, maintaining a healthy weight (BMI 18.5–24.9), quitting smoking, and supplementing with folic acid, vitamin D (600 IU/day) and coenzyme Q10 (200–300 mg/day) can help. Relaxation techniques, yoga or therapy reduce stress and support a more balanced hormonal environment. These habits are supportive but don’t replace assisted reproduction treatment if ovarian reserve is low. When Should I Do Preimplantation Genetic Testing? PGT is recommended if you’ve had recurrent miscarriages, are over 35, or have genetic diseases in the family. Testing the embryo before transfer reduces the risk of chromosomal abnormalities and improves implantation rates. What Is Egg Donation for? Egg donation is an alternative when your own eggs aren’t viable. Eggs from young donors have better chromosomal quality and mitochondrial energy, increasing the chances of a successful pregnancy. At Ingenes we ensure rigorous selection, compatibility and emotional support. How Do Age and Hormones Affect Oocyte Quality? After 35, egg quantity and quality decline due to DNA wear and reduced mitochondrial function. High FSH levels (>10 mIU/ml on day 3) and low AMH (

Uterine myomatosis is the formation of myomas or fibroids inside the uterus. These are benign tumors classified according to their location. Depending on where they are found, fibroids are classified as: Intramural: within the muscular wall of the uterus. They can affect fertility if they exceed 4 cm. Submucosal: on the surface of the uterine lining. They hinder embryo implantation. Subserosal: in the outer layer of the uterus. They usually do not interfere with fertility. What is uterine myomatosis and why does it matter for fertility? Uterine myomatosis involves the growth of fibroids, benign smooth muscle tumors, inside the uterus. It affects about 20% of women of reproductive age, especially after age 30. Fibroids can range from microscopic nodules to masses over 4 kg, altering the shape of the uterus and reducing pregnancy chances. How common is uterine myomatosis in those trying to conceive? Uterine fibroids are the most common pelvic tumors in women of reproductive age, present in nearly 70–80% before menopause. Although many are asymptomatic, those that deform the uterine cavity—particularly large intramural and submucosal fibroids—are involved in up to 80% of uterine factor infertility cases. How do fibroids affect embryo implantation? Large submucosal and intramural fibroids can: Alter sperm transport and uterine peristalsis Reduce endometrial receptivity by compressing the lining Increase the risk of implantation failure and early miscarriage Can fibroids complicate pregnancy? Yes. During pregnancy, fibroids can cause: Higher risk of miscarriage and preterm birth Fetal growth restriction due to lack of space Cervical canal obstruction or labor dystocia Postpartum hemorrhage from poor uterine contraction What symptoms may indicate fibroids? About 25% are asymptomatic. When symptoms occur, they include: Sensation of pelvic pressure or heaviness Heavy or prolonged menstrual bleeding Pelvic cramps and irregular bleeding Frequent urination or difficulty urinating Secondary infertility or recurrent miscarriages Severity depends on fibroid size, number, and location. How is diagnosis confirmed? Transvaginal ultrasound is the gold standard, with nearly 100% sensitivity (95% transabdominal). In complex cases, MRI is used. Always consult a reproductive medicine specialist to interpret results and design a treatment plan. Fertility-preserving treatment options Choice depends on age, fibroid characteristics, and reproductive goals: Expectant management for small, asymptomatic fibroids Myomectomy (surgical removal), followed by assisted reproduction techniques Controlled ovarian stimulation combined with in vitro fertilization (IVF) if cavity distortion persists IVF bypasses uterine transport obstacles and allows for selecting the embryo with the highest implantation potential. For more information, see our guide on Endometriosis: what it is and how it impacts fertility. FAQ 1. Can small fibroids disappear on their own? Yes. Many remain stable or shrink after menopause due to estrogen decline. In reproductive age, asymptomatic fibroids under 2 cm are usually monitored with periodic ultrasounds. If you plan to conceive, even a small submucosal fibroid can affect implantation, so consult your doctor to assess intervention before trying to conceive. 2. Are there non-surgical treatments? GnRH agonists and selective progesterone receptor modulators can temporarily shrink fibroids and reduce bleeding in 3–6 month cycles. They improve conditions before surgery or comfort but are not definitive solutions. Never self-medicate without medical supervision. 3. When can I attempt IVF after a myomectomy? Ideally between 6 and 12 months after surgery, before recurrence risk increases. This timing allows the uterine lining to heal and optimizes pregnancy chances. Make sure your specialist confirms proper healing with ultrasound or hysteroscopy before starting treatment. 4. Does the risk of miscarriage increase? Yes. Fibroids that deform the cavity or alter blood flow are associated with early pregnancy loss. Risk increases with fibroid size and location, especially submucosal and large intramural fibroids. Proper management, surgical or with assisted reproduction, significantly reduces miscarriage rates. Always consult a specialist before making decisions. References Faerstein, E., Szklo, M., & Schwingl, P. J. (2001). Risk factors for uterine leiomyoma: a practice-based case–control study. American Journal of Epidemiology, 153(5), 463–469. doi:10.1093/aje/153.5.463 Lau, W., & Shlisselberg, S. (2016). Management of uterine fibroids. American Family Physician, 94(2), 106–113. https://www.aafp.org/afp/2016/0715/p106.html MedlinePlus. (2021). Uterine fibroids. https://medlineplus.gov/uterinefibroids.html Stewart, E. A. (2015). Uterine fibroids. Lancet, 376(9745), 145–157. doi:10.1016/S0140-6736(10)60246-1 Remember: every body is unique. Stay informed, keep hope, and consult an assisted reproduction specialist for personalized care.

Low ovarian reserve is a condition that impacts a woman’s fertility, characterized by a reduced number and lower quality of eggs in the ovaries. Although it usually appears after age 35, genetic, environmental factors and certain diseases can accelerate this process in younger women. What is low ovarian reserve and how does it affect fertility? Ovarian reserve measures how many viable eggs (oocytes) you have. We are born with a limited number and, over time, both quantity and quality decline. When the antral follicles detected by ultrasound are few and the antimüllerian hormone (AMH) in blood is low, the chances of conceiving naturally decrease and assisted reproduction may be necessary. Why is ovarian reserve important for conception? Knowing your ovarian reserve helps you plan your path to motherhood or fatherhood more effectively. A healthy reserve generally responds well to stimulation treatments, producing more mature eggs for fertilization, whether naturally or via in vitro fertilization, and improves successful pregnancy rates. What causes low ovarian reserve? Some factors can accelerate egg loss: Advanced age: After 35, egg quality and quantity decline more rapidly. Genetic factors: FMR1 gene premutations or premature ovarian insufficiency reduce reserve. Medical treatments: Chemotherapy or pelvic radiation can damage the ovaries. Ovarian surgery: Removing cysts or endometriomas removes healthy follicles. Autoimmune diseases: Lupus or thyroid disorders affect ovarian function. How is low ovarian reserve diagnosed? The following are used to confirm this diagnosis: Hormonal tests: FSH >10 IU/L on day 3 of the cycle or AMH

Discover the key differences between menstruation and implantation bleeding. Learn to recognize the first signs of pregnancy and better understand your menstrual cycle with clear, approachable information. At Ingenes, we’re by your side every step of the way toward parenthood, offering personalized guidance and care. Understanding menstruation and implantation bleeding is essential whether you’re trying to conceive or simply getting to know your body. Although both involve bleeding, they are distinct processes with their own signs. What is menstruation? Menstruation is the shedding of the uterine lining when there’s no fertilized egg. A regular cycle (every 21–35 days) usually reflects hormonal balance and good reproductive health. Duration: 3–7 days. Flow: Light to heavy, sometimes with clots. Color: Bright red to dark brown. Symptoms: Cramps, bloating, mood swings, and fatigue. What is implantation bleeding? When the fertilized egg attaches to the uterus, very light bleeding may occur, called implantation bleeding. It’s often one of the first signs of pregnancy. Timing: 10–14 days after conception, around the expected period date. Duration: 1–2 days. Flow: Very light. Color: Pale pink or brown. Key differences 1. Calendar If you track your cycle, spotting outside your usual window may indicate implantation. 2. Intensity and Symptoms Menstruation is heavier and may come with strong cramps. Implantation is light and nearly painless. 3. Appearance of the Flow Bright red flow = menstruation. Pink or brown spotting = implantation. Knowing these signs helps you understand your body and take informed next steps. For more details, visit Implantation Bleeding: What You Need to Know. When to seek medical help? If bleeding is very heavy, accompanied by severe pain, or you notice unusual spotting, see a reproductive medicine specialist. At Ingenes, we provide comprehensive evaluations to rule out issues like ectopic pregnancy, hormonal imbalances, or uterine abnormalities. Early assessment improves your chances of a healthy pregnancy. Frequently Asked Questions 1. Can You Have Implantation Bleeding Without Pregnancy? No. That bleeding happens when the embryo implants. Spotting outside your cycle usually stems from hormones or irritation. If in doubt, take a test after a missed period and consult if spotting continues. 2. Is Mild Cramping Normal? Light cramps can occur with implantation, but if pain is severe, seek medical attention. 3. Do Contraceptives Affect Bleeding? After stopping them, your cycle may be irregular and spotting might be mistaken for implantation. Track your cycle and talk to your doctor if spotting lasts more than two months or is painful. 4. Is Bleeding a Reliable Sign of Pregnancy? Not on its own. Many women don’t experience it. Pregnancy tests and hCG analysis are more accurate and help rule out issues like ectopic pregnancy. Sources MedlinePlus. (2023). Menstruation. https://medlineplus.gov/menstruation.html ACOG. (2022). Early Pregnancy Bleeding. https://www.acog.org/womens-health/faqs/early-pregnancy-bleeding Britannica. (2021). Implantation. https://doi.org/10.1036/1097-8542.747900 NIH. (2020). Implantation Bleeding. https://www.ncbi.nlm.nih.gov/books/NBK538507/ We’re with you every step of the way. If you have questions or want personalized guidance, consult an assisted reproduction specialist. Your journey to parenthood deserves expert care and close support.

World Prostate Cancer Day, observed every June 11, reminds us how important it is to take care of ourselves and detect this common men’s disease early. It’s an opportunity to learn about prevention, early detection, and treatments aimed at improving quality of life. What is prostate cancer and how does it develop? Prostate cancer arises when cells in this gland begin to grow uncontrollably. It’s the most common cancer in men and often goes unnoticed in its early stages. That’s why early detection through screening significantly increases the chances of successful treatment. The importance of early detection A simple PSA blood test and a digital rectal exam can reveal changes before you notice symptoms. If you’re over 50 or have a family history, talk to your doctor about scheduling screening. In some cases, and always under medical supervision, 5-alpha reductase inhibitors help reduce risk. Symptoms and warning signs In advanced stages you may experience difficulty urinating, weak flow, blood in urine or semen, and pelvic or lower back pain. If you notice any of these signs, avoid self-medicating and seek professional care as soon as possible. Risk factors Your age (over 50), having a first-degree relative diagnosed, being of African American descent, a high-fat diet, obesity, and certain occupational exposures increase risk. A healthy lifestyle—balanced diet, moderate exercise at least 150 minutes a week, and quitting smoking—can make a difference. Prevention with healthy habits A diet rich in fruits, vegetables, and whole grains, low in red meat and saturated fats, along with maintaining a healthy BMI and regular exercise, helps protect your prostate. Always consult your doctor before taking supplements or making drastic dietary changes. Treatment options Treatment varies depending on cancer stage, your age, and preferences. It may include active surveillance, surgery (prostatectomy), radiotherapy, hormone therapy, chemotherapy, or a combination. If you’re trying to increase your chances of pregnancy, it’s essential to consult a reproductive specialist before deciding on any treatment. World Prostate Cancer Day invites us to take control of our health. Stay informed, get regular check-ups, and adopt a healthy lifestyle. At Ingenes we’re with you: check our special resources and expert articles to learn more. Frequently Asked Questions (FAQ) 1. When should PSA testing begin? Most guidelines recommend starting at age 50. If you have a family history or belong to a higher-risk group (African Americans), begin at 45. PSA measures prostate antigen in blood; values above 4 ng/mL often require further tests like transrectal ultrasound or biopsy. A high result doesn’t always mean cancer, so interpret data with a specialist. 2. Side effects of radiotherapy It can cause fatigue, bladder irritation, increased urination, and mild diarrhea. In some cases, erectile dysfunction or urethral stricture may occur, but these are usually temporary and manageable with medication or sexual therapy. Discuss with your oncologist and follow recommendations to minimize effects. 3. How effective is active surveillance? For low-risk or slow-growing cancers, it involves periodic PSA monitoring, physical exams, and biopsies. Over 80% of patients avoid aggressive treatment for at least 10 years. It requires commitment to appointments and healthy habits, allowing treatment initiation if the disease progresses. 4. Dietary influence Saturated fats and red meat may increase advanced prostate cancer risk. In contrast, tomato lycopene, broccoli sulforaphane, and green tea catechins offer protection. A Mediterranean pattern—olive oil, fish, fruits, and vegetables—is linked to lower incidence. Consult a nutritionist to adapt this diet to your life. Sources National Cancer Institute. (2023). Prostate-Specific Antigen (PSA) Test. https://www.cancer.gov/types/prostate/psa-fact-sheet American Cancer Society. (2022). Prostate Cancer Early Detection. https://doi.org/10.3322/caac.21684 MedlinePlus. (2023). Prostate Cancer. https://medlineplus.gov/prostatecancer.html World Health Organization. (2021). Cancer prevention. https://www.who.int/news-room/fact-sheets/detail/cancer Remember that each body is unique. You have our support—don’t hesitate to consult a reproductive specialist to address your concerns and receive the guidance you need.

Ingenes Mazatlán nació para ayudar a que más personas cumplan su sueño de tener un bebé con apoyo de la Reproducción Asistida.

World Health Day invites us to consider all the factors that influence having a child. From our physical health and lifestyle to environment and socioeconomic conditions, every detail counts. Understanding how these aspects combine can make a difference when building a family. How does physical health affect fertility? Physical health of both partners is essential to conceive and carry a pregnancy to term. Conditions like obesity (BMI >30 kg/m²), type 2 diabetes, thyroid disorders or STIs can damage eggs and sperm. After age 35, ovarian reserve declines and sperm quality decreases by 1–2 % each year. Avoid self-medication and always seek professional guidance. Before taking supplements or medications, consult an assisted reproduction specialist. Early and personalized diagnosis increases your chances of success. How does lifestyle affect your chances of conceiving? Smoking, consuming more than 14 units of alcohol per week or using illicit drugs can damage the DNA of eggs and sperm. A diet rich in folates, omega-3 and vitamins D and E promotes a healthy uterine environment and sperm quality. Doing at least 150 minutes of moderate exercise weekly helps balance hormones. Relaxation techniques like yoga or mindfulness also reduce stress and support ovulation and spermatogenesis. What impact does environment have on your reproductive capacity? Pollution and exposure to toxins (phthalates, pesticides) can lower sperm count and disrupt ovarian function. Chronic stress raises cortisol, hindering reproductive hormone production. Improve your surroundings: ensure good ventilation, get enough sleep and minimize household pollutants to protect your fertility. Why do socioeconomic factors matter in the decision to become a parent? Having economic stability and access to quality healthcare influences when you decide to have children and how many. Job or social insecurity often delays parenthood or limits family size. Education and reliable information allow you to plan freely and confidently. Rely on official sources to make informed decisions. How does mental health affect your fertility? Anxiety and depression reduce libido and can disrupt the menstrual cycle. Facing fertility challenges without emotional support increases psychological strain. Seeking psychological support at fertility centers strengthens your resilience and improves treatment adherence. What advances does assisted reproduction offer today? Techniques such as in vitro fertilization (IVF) and artificial insemination have helped many couples. However, their cost (between 8,000 and 15,000 USD per cycle) and emotional impact require robust support. Learn more in World Sexual Health Day: A Holistic View of Wellness and Fertility and World Fertility Day: A Date to Inform, Empathize, and Never Lose Hope. On this World Health Day, let’s commit to habits and environments that nurture our reproductive health. With information, empathy and comprehensive care, we can support you at every step toward parenthood. Frequently Asked Questions (FAQ) 1. What Is the Best Age to Conceive? The ideal range is usually between 20 and 30 years, when ovarian reserve and egg quality are optimal. After 35, fertility declines and the risk of genetic abnormalities increases. Every body is unique. An assisted reproduction specialist will help you evaluate hormones like AMH and FSH to plan more safely. 2. How Does Body Weight Affect Fertility? A BMI below 18.5 or above 30 can disrupt menstrual cycles and sperm quality. Fat tissue produces estrogens that unbalance hormones. A personalized nutrition plan under medical supervision helps reach a healthy BMI and increases your chances of conceiving. 3. What Diagnostic Tests Are Recommended Before Trying to Get Pregnant? Ideally, a hormonal profile (FSH, LH, AMH, TSH), a semen analysis and tubal patency studies (hysterosalpingography). These tests identify potential obstacles early. It’s also advisable to assess ovarian reserve and conduct a general health check—thyroid profile, glucose and liver function—to design a successful reproductive plan. 4. Is Psychological Support Necessary During Assisted Fertility? Yes. Stress and anxiety can lower implantation rates and affect your well-being. Psychological help improves treatment adherence and provides emotional tools at each stage. Support groups, individual or couple therapy and relaxation techniques are valuable complements to strengthen your reproductive journey. Sources American Society for Reproductive Medicine. (2020). Practice Committee guidelines. Reproductive Medicine. doi:10.1016/j.fertnstert.2020.03.028 MedlinePlus. (2023). Infertility: Overview. https://medlineplus.gov/infertility.html World Health Organization. (2021). Reproductive health indicators. https://www.who.int/reproductive-health/ Practice Committee of the American Society for Reproductive Medicine. (2015). Testing and interpreting semen analysis in infertility evaluation. Fertility and Sterility, 103(3), e18–e25. doi:10.1016/j.fertnstert.2015.01.016 Remember that every story is unique. For personalized support and answers to your questions, consult an assisted reproduction specialist. You are not alone on this journey!

Assisted reproduction treatments often require a significant financial investment, especially high-complexity ones like in vitro fertilization. At Ingenes Institute you can save because our laboratories are in Mexico. This way, you start your treatment in the U.S. and complete it in Mexico. How does the treatment between Mexico and the U.S. work? Your high-complexity process consists of two stages: Initial evaluation: at your first appointment we perform lab tests and ultrasounds to design the ideal protocol. Trip to Mexico: there we retrieve your eggs (when follicles measure 17–20 mm), prepare the semen sample (yours or donor’s), and carry out the embryo transfer. Thanks to the alliance between Ingenes USA and Mexico, we use NASA technology that keeps your samples (eggs, sperm, and embryos) at –196 °C in liquid nitrogen tanks. Ingenes Labs Star at Home Multicycle Program: your advantages With up to 4 IVF cycles, our program maximizes your chances of pregnancy. Each package includes: Personalized follow-up by an embryologist Access to egg and sperm bank Embryo cryopreservation for up to 1 year Consultations, ultrasounds, pregnancy tests, and medical analyses Embryo preparation and Assisted Hatching Do not self-medicate. Before starting, consult a reproductive specialist to adjust doses and protocol. Ingenes Mexicali: your best option on the southern border Ingenes Mexicali offers a warm, intimate environment, perfect for relaxing and taking care of your emotional health. With over 4 million American tourists per year, the city combines rest and support before embryo transfer. Dr. Felipe Camargo Dr. Felipe Camargo, obstetrician-gynecologist from the University of Rosario and an expert in infertility and genetics with over 20 years of experience and a Master’s in Human Reproduction (University of Valencia), leads our protocols. At Ingenes we are committed to your dream of becoming parents. Ready to take the next step? Frequently Asked Questions (FAQ) 1. What is IVF and what is it for? In vitro fertilization (IVF) is a technique where eggs and sperm are joined in a laboratory at 37 °C. It helps couples with blocked tubes, low ovarian reserve (AMH < 1 ng/mL), severe male factors (TMC < 5 million/mL), advanced endometriosis, or recurrent implantation failures. 2. How much does an IVF cycle cost in Mexico compared to the U.S.? In the U.S. a cycle ranges from 15,000–20,000 USD. In Mexico, thanks to subsidies and lower costs, it can be between 6,000–8,000 USD. Our combined packages can save you up to 50%. With laboratories near the border and the option to complete your treatment in the U.S. and Mexico, you save time and travel procedures. 3. What risks are involved in traveling to Mexico for fertility treatment? Traveling to Mexico is safe if you follow biosafety protocols and transport in liquid nitrogen tanks. Ingenes holds ISO 9001 and CAP certifications to guarantee quality and chain of custody. Plan your trip in advance, check immigration requirements, and carry your medication in your carry-on with a prescription. 4. What success rate does Ingenes offer in combined treatments? We report cumulative rates above 60% in multicycle programs of up to 4 cycles. These figures vary according to age, ovarian reserve, and semen or donor quality. Our personalized approach and advanced technology (time-lapse, PGD/PGS) improve embryo viability and reduce the risk of miscarriage. Sources consulted American Society for Reproductive Medicine. Practice Committee reports. Fertility and Sterility. 2021. Centers for Disease Control and Prevention. Assisted Reproductive Technology (ART). 2022. MedlinePlus. In Vitro Fertilization. U.S. National Library of Medicine. 2021. World Health Organization. WHO Laboratory Manual for the Examination and Processing of Human Semen. 6th ed. 2020. Your desire to become a mother or father is valuable. We are here to support you every step of the way. Consult a fertilization specialist and refresh yourself with the best professional guidance.

At Ingenes, every success is born from the hope, strength, and love of our families. That’s why the recent gathering at Ingenes Tijuana was so special: several moms reunited with their babies to capture, in a photo session, their fulfilled dream. This year 2025 has an even more emotional flavor: we celebrate 20 years of making the extraordinary possible. Two decades supporting women and couples to have the baby they long for. What does this celebration at Ingenes Tijuana mean? More than a photo session, it was the final chapter of a journey full of doubts that ended in the joy of holding their babies. With genuine laughter and curious little eyes, each image reflects our moms’ resilience and courage. By reaching 20 years in 2025, we reaffirm our track record of excellence, from In Vitro Fertilization (IVF) to fertility preservation with egg vitrification, following personalized protocols and precise dosages in mL and µg to optimize every treatment. How did the moms connect in Tijuana? Beyond the photos, the gathering allowed them to share real assisted reproduction stories, offering support and empathy to those still on the journey. It was a demonstration that although each case is unique, all share the deep desire to start a family. Each baby present symbolizes our team’s dedication and the trust placed in Ingenes, an institute that combines cutting-edge technology with a human commitment to make thousands of dreams come true. The legacy of hope from this gathering We know every success story inspires many others. These photos not only capture magical moments but also encourage those still seeking parenthood. Avoid self-medication: before making any decision, always consult a reproductive medicine specialist. As we celebrate our 20th anniversary, we reaffirm our commitment to accompany you every step of the way, with comprehensive solutions and a team that puts its heart into every case. Ingenes Tijuana services for your dream of becoming parents Located near the border, Ingenes Tijuana serves patients from Mexico and the United States with advanced treatments: Intrauterine Insemination (IUI), Preimplantation Genetic Testing (PGT), and fertility preservation. Each plan is tailored to your needs with state-of-the-art technology. If your dream is to become a mom or dad, discover why Ingenes San Diego and our Surrogacy program in Mexico are benchmarks in professionalism and warmth. Frequently Asked Questions 1. Recommended age for a fertility treatment Ideally before age 35, since egg quantity and quality decline over time. But each case is different: your medical history, ovarian reserve (AMH and antral follicles), and lifestyle determine the best plan. Before deciding, get a transvaginal ultrasound and hormonal tests. Do not self-medicate: a specialist will prescribe the precise dosages in IU and µg and the appropriate protocol. 2. Differences between IUI and IVF Intrauterine Insemination (IUI) places prepared sperm in the uterus after mild stimulation. It’s less invasive, with lower medication costs and dosages (75–150 IU of gonadotropins). In Vitro Fertilization (IVF) retrieves eggs, fertilizes them in the lab, and transfers embryos. It offers higher success in complex cases and allows PGT to reduce genetic risks. 3. Lifestyle and fertility A diet rich in omega-3, moderate exercise, and not smoking improve egg and sperm quality. Maintaining a BMI between 18.5 and 24.9 kg/m² optimizes response to stimulation. Stress can affect the hypothalamic-pituitary-ovarian axis and reduce ovulation. Relaxation, therapy, and support groups like Ingenes Moms help maintain overall well-being. 4. Risks of assisted reproduction Main risks include ovarian hyperstimulation syndrome (OHSS), multiple pregnancies, and invasive procedure complications. OHSS is managed by adjusting gonadotropin dosages and monitoring estradiol (pg/mL) and follicles. With an experienced team and personalized protocols, risks decrease. Before starting, see a specialist and avoid self-medication. Sources American Society for Reproductive Medicine. (2021). Practice Committee Guidelines. https://www.asrm.org MedlinePlus. (2024). Fertility treatments. https://medlineplus.gov/fertilitytreatments.html World Health Organization. (2020). WHO laboratory manual for the examination and processing of human semen (6th ed.). https://doi.org/10.18356/9789241547789 ESHRE. (2022). Good Practice Recommendations on Ovarian Stimulation. Human Reproduction Open, 2022(3), hoac030. https://doi.org/10.1093/hropen/hoac030 On this journey, you are not alone: you have our support. Always consult a reproductive specialist to find the best option and be accompanied with the experience you deserve.

Why is Guadalajara an ideal place to have your baby? This city is one of the most important in Mexico thanks to its economic infrastructure and high technological development with world class innovations.

Every year, during the third week of June, we celebrate International Men’s Health Week: a time to care for men’s physical, mental and emotional well-being. On this date—created to raise awareness of conditions that affect men—we also take the opportunity to talk about a topic surrounded by myths and silence: male reproductive health. At Ingenes we know fertility isn’t just a women’s issue. In 50% of infertility cases in couples, a male factor is involved, either alone or along with other factors. That’s why we believe this week is ideal for breaking taboos, offering clear information and opening doors to real solutions. What is International Men’s Health Week and why does it matter for fertility? This week puts the focus on problems that often go unmentioned, including men’s reproductive health. By discussing sperm quality, hormonal balance and lifestyle habits, we empower men and couples to seek evaluations and treatments in time. How do male factors influence a couple’s fertility? Male fertility depends on sperm concentration (million/mL), motility (%), morphology (% normal forms) and semen volume (mL). A low count (<15 million/mL), reduced motility (<40%) or abnormal morphology (<4%) decrease the chances of conception. In addition, hormonal imbalances—such as low testosterone (<300 ng/dL)—and structural issues like varicocele also have an impact. What tests diagnose male fertility problems? The first step is a semen analysis that measures: Sperm concentration (million/mL) Motility (% of motile sperm) Morphology (% of sperm with normal form) Semen volume (mL) If the results are out of range, additional studies are performed: hormonal panel (FSH, LH, testosterone), genetic tests and ultrasound to detect underlying causes. What lifestyle changes improve sperm quality? Small adjustments make a difference: Quit smoking and moderate alcohol consumption Maintain a healthy weight (BMI 18.5–24.9 kg/m²) Follow a balanced diet rich in antioxidants (vitamin C, E, zinc) Manage stress with exercise or relaxation practices Avoid excessive heat (saunas, hot tubs) and exposure to toxins Does a man’s age affect his fertility? Although men produce sperm throughout their lives, quality declines with age. After 40, motility and morphology may worsen, and the risk of DNA fragmentation and genetic mutations increases. Advanced paternal age is associated with higher risks of miscarriage and certain disorders in offspring. How to preserve male fertility for the future? Sperm cryopreservation is the best option. By freezing semen samples at –196 °C in liquid nitrogen, fertility is protected before medical treatments (chemotherapy, radiation) or age-related decline. At Ingenes we offer secure storage and easy access when you need it. What treatments are available for male infertility? Most cases are treatable. Options include: Lifestyle interventions: diet, exercise and stress management Medical therapy: antibiotics for infections, hormonal treatments Surgery: varicocelectomy, vasectomy reversal, blockage removal Assisted reproduction: IUI, IVF, ICSI or PICSI to select the best sperm For a comprehensive approach, visit our article World Sexual Health Day: A Holistic View of Wellness and Fertility and learn more about paternal health in Father’s Month: Male Reproductive Health and Everyone’s Right to Build a Family. Why does mental health matter in male fertility? Emotional well-being influences hormonal balance and semen parameters. Anxiety and depression can lower testosterone (<300 ng/dL) and affect libido and sexual function. At Ingenes we offer psychological support to accompany men and couples during the fertility process. Talking openly and having support networks encourage testing and proactive measures. Celebrating men’s health this week is not a sign of weakness, but a brave step toward building the family you dream of. Frequently Asked Questions 1. Which lifestyle habits impact male fertility the most? Quitting smoking and moderating alcohol are key changes. Tobacco damages sperm DNA and reduces motility and count. Excessive alcohol disrupts hormonal balance, lowers testosterone and affects spermatogenesis. Regular exercise, a diet rich in antioxidants (vitamin C, E, zinc) and stress-reduction techniques (meditation, yoga), plus maintaining a healthy BMI (18.5–24.9 kg/m²), also support fertility. 2. How do hormonal imbalances affect male fertility? Hormones like FSH, LH and testosterone regulate sperm production in the testes. Low testosterone (<300 ng/dL) leads to reduced libido, erectile dysfunction and poor sperm formation. High FSH or LH levels may indicate testicular failure or pituitary issues. Blood tests diagnose these imbalances and they are treated with testosterone replacement, gonadotropins or specific medications under supervision. 3. When should a couple consider a semen analysis? If they have tried to conceive for more than 12 months without success—or 6 months if the woman is over 35—it is recommended. Early evaluation speeds up diagnosis and opens treatment options. Even before trying, men with risk factors (infections, varicocele, toxin exposure, chronic diseases) can get tested to improve or preserve their fertility. 4. Are there risks to sperm cryopreservation? Sperm freezing is a safe, routine procedure. Collection may cause slight discomfort, but the freezing process preserves long-term viability. The main considerations are storage costs and proper sample identification. At specialized banks like Ingenes we follow international protocols to ensure sperm integrity upon thawing. References American Urological Association. (2018). Evaluation and Management of Infertility in Men. https://www.auanet.org/guidelines World Health Organization. (2021). WHO laboratory manual for the examination and processing of human semen (6th ed.). Geneva: WHO Press. O’Flynn O’Brien, K. L., Vargha, A., & Agarwal, A. (2010). The genetic causes of male factor infertility: a review. Human Reproduction Update, 16(4), 331–344. https://doi.org/10.1093/humupd/dmp051 National Center for Biotechnology Information. (2022). Male Infertility. In StatPearls. https://www.ncbi.nlm.nih.gov/books/NBK279026/ Remember: every body is unique. If you have concerns about your fertility, seek guidance from an assisted reproduction specialist. We are here to accompany you on your path to fatherhood.

Why is Monterrey an ideal place to have your baby? It is one of the most important cities in Mexico, and it is located in the northwest of the country. It is considered the industrial pole thanks to the fact that there are Mexican global companies, as well as the best rated universities in Latin America.

Thinking about coming to Ingenes TJ? Meet the most visited city in the world. Each year, more than 50 million people cross between Tijuana and San Diego, and it is classified as a global city for being a commercial cultural center in North America.

Ingenes Querétaro is one of the branches of the leading Institute of Fertility and Genetics in Latin America. The state of Querétaro has stood out thanks to its economic dynamics. In recent years, the development of the entity has excelled thanks to the aerospace industry.

During pregnancy, anemia is very common. The mother’s body needs more iron to produce red blood cells that carry oxygen to the baby and to her own tissues. If you don’t consume enough iron, your stores become depleted and hemoglobin drops, causing anemia. Symptoms may include extreme fatigue, weakness, dizziness, palpitations, pale skin, and shortness of breath, especially in the third trimester. Anemia also increases the risk of preterm birth and low birthweight. Preventing and treating anemia is essential for both mother and baby. Below, Dr. Edith María Ramos Reyes explains its causes, risk factors, and the best treatment options: dietary changes, iron supplements, and, in severe cases, transfusions. What is anemia in pregnancy and why does it occur? Gestational anemia is diagnosed when hemoglobin is below: <11 g/dL in the first and third trimesters, <10.5 g/dL in the second trimester. During pregnancy, blood volume increases by up to 50%, so about 30 mg of iron daily is needed. If you don’t meet this demand through diet, your stores will be exhausted. Mild: 10.1–10.9 g/dL Moderate: 7.1–10 g/dL Severe: <7 g/dL Risk factors and symptoms Multiple pregnancies, short intervals between pregnancies, low‐iron diets, or chronic diseases (such as kidney problems) increase the risk. Common symptoms include: Fatigue and weakness Dizziness and palpitations Pale skin and brittle nails Shortness of breath during activity Only a blood test can confirm the diagnosis; that’s why good prenatal care is crucial. Prevention: Diet and Supplements Include heme iron (lean meat, liver) and non‐heme iron (legumes, leafy greens) in your diet, paired with vitamin C to improve absorption. Avoid taking calcium at the same time as iron. Practical recommendations: 30 mg of elemental iron daily on an empty stomach 500 mL of orange juice daily with meals 100 g of spinach and 150 g of lentils per week Do not self‐medicate; always consult your doctor. Treatments by severity For mild to moderate anemia: Oral iron supplements (30–60 mg Fe²⁺ daily) Fortified foods and diet therapy In severe anemia (<7 g/dL) or with cardiac symptoms, a red blood cell transfusion under obstetric and hematological supervision may be necessary. Ingenes Support At the Ingenes Maternal-Fetal Medicine Unit, with over 15,000 pregnancies managed, we provide early detection and personalized prevention and treatment plans for you and your baby. FAQ: Frequently Asked Questions 1. Does anemia affect fetal development? Yes. If severe, there is a risk of preterm birth and low birthweight because the fetus receives less oxygen. Timely diagnosis and treatment with iron, along with good prenatal follow‐up, reduce these complications. 2. Is it safe to take iron supplements throughout pregnancy? Generally yes, as long as you’re supervised by a specialist. You start with 30 mg/day and adjust based on your hemoglobin levels and tolerance. If you experience side effects (constipation, nausea), you can change the formulation or split the dose. 3. Which foods help absorb iron better? Vitamin C enhances non‐heme iron absorption. Add citrus fruits, strawberries, or peppers to your iron‐rich meals, and avoid tea, coffee, or calcium‐rich foods at the same time. 4. Is a transfusion always necessary in severe anemia? Not always. The decision depends on your symptoms, hemoglobin level, and how quickly it drops. If you tolerate oral or intravenous iron treatments, these are preferred over transfusion. However, in cases of cardiovascular or fetal risk, transfusion is the fastest and safest option. Sources World Health Organization. (2021). Anaemia. https://www.who.int/health-topics/anaemia#tab=tab_1 American College of Obstetricians and Gynecologists. (2020). Practice Bulletin No. 233: Screening and Management of Iron Deficiency Anemia. NIH Office of Dietary Supplements. (2022). Iron Fact Sheet for Health Professionals. MedlinePlus. (2023). Iron Deficiency Anemia. Remember that every body is unique. If you have questions or want to improve your chances of a healthy pregnancy, see a reproductive medicine specialist. We’re with you on this journey!

HTown Best shares expert reviews and opinions so patients receive satisfying experiences and have their needs met. What is Ingenes Houston and why does HTown Best recognize it? Ingenes Houston is a leading assisted reproduction clinic that supports women and men on their journey to parenthood. Recently, the Ingenes Institute was highlighted by HTown Best as a member of the McAllen Chamber of Commerce in Texas. This recognition is based on our use of advanced IVF techniques and personalized care: we maintain success rates above 60% per cycle and provide continuous emotional support. How does HTown Best evaluate assisted reproduction clinics? HTown Best is a Houston network that combines local opinions and expert criteria to rate services. Its parameters include: Live birth rate per embryo transfer (LBR/ET). Patient satisfaction score, obtained via surveys. Technological standards: time-lapse incubators, PGT-A genetic screening on day 5 post-fertilization. Clinic accreditations and staff certifications. By combining quantitative data (for example, 12–15 oocytes retrieved per cycle) and qualitative feedback, HTown Best highlights only those clinics with proven results and close care. Why choose a locally recommended fertility clinic in Houston? The Houston specialist community offers personalized treatments: from intrauterine insemination (IUI) with 0.5–1 mL of sperm suspension to ICSI with microinjection of a single sperm. A clinic endorsed by residents and experts guarantees: State-of-the-art laboratories. Multidisciplinary teams: reproductive endocrinologists, embryologists, and psychologists. Flexible financing plans to cover medications (300–500 IU of gonadotropins daily). At Ingenes Houston we collaborate with international partners, such as our team in California—learn more here—to bring the most innovative protocols. What to expect at the first consultation? At your first visit we review your medical history, perform a transvaginal pelvic ultrasound (7.5 MHz probe) and a hormonal panel (FSH, LH, AMH in ng/mL). We design a customized IVF or IUI protocol and discuss lifestyle habits. Avoid self-medication and always consult an assisted reproduction specialist if you want to increase your chances of pregnancy. Frequently Asked Questions (FAQ) 1. How does Ingenes Houston improve success rates? We use time-lapse incubators and PGT-A to select euploid embryos and maximize implantation. Additionally, we adjust ovarian stimulation based on AMH and AFC. We offer psychological support and support groups: studies show that low cortisol levels favor endometrial receptivity. 2. What are the differences between IUI and IVF? IUI deposits 0.5–1 mL of selected sperm into the uterus during ovulation. It is less invasive and costs less, with pregnancy rates of 10%–20% per cycle. IVF fertilizes eggs in the lab and transfers one or more embryos, reaching 50%–60% success. The choice depends on age, ovarian reserve, and sperm quality. In cases of severe male factors or IUI failures, IVF is usually the best option. 3. When should ovarian reserve be evaluated? It is recommended from age 35 or after 6 months of not conceiving naturally. The test measures AMH in ng/mL and AFC by ultrasound. AMH > 1.2 ng/mL and AFC > 7 follicles indicate good reserve. With AMH < 0.7 ng/mL, we consider egg donation or vitrification. 4. What role does lifestyle play? A BMI between 18.5 and 24.9, moderate caffeine intake (< 200 mg/day), and not smoking increase the chances. Moderate exercise (30 min daily) regulates hormones and improves receptivity. We recommend a diet rich in omega-3, vitamin D, and 400 µg/day of folic acid. Psychological support reduces anxiety and favors outcomes. Sources American Society for Reproductive Medicine. (2020). Practice Committee guidelines on assisted reproductive technology. Fertility and Sterility. https://doi.org/10.1016/j.fertnstert.2020.03.010 National Library of Medicine. (2022). Anti-Müllerian Hormone Testing. MedlinePlus. https://medlineplus.gov/lab-tests/anti-mullerian-hormone-test/ La Marca, A., & Sunkara, S. K. (2014). Individualization of controlled ovarian stimulation in IVF using ovarian reserve markers. Human Reproduction Update, 20(1), 124–140. https://doi.org/10.1093/humupd/dmt039 Kovalevsky, G., & Crosignani, P. (2017). Impact of lifestyle factors on IVF outcomes. Reproductive BioMedicine Online, 34(5), 567–575. https://doi.org/10.1016/j.rbmo.2017.02.002 We are with you every step of this journey. If you dream of becoming a mom or dad, don’t hesitate to seek specialized assisted reproduction help.

In a society where turning 40 without a partner but with the dream of becoming a mother may seem challenging, we want to remind you that this stage is not the end, but the beginning of a journey full of hope. Here you will find clear and approachable information about your fertility options and how Ingenes accompanies you step by step. How does being 40 affect my fertility and what can I do? At 40, ovarian reserve decreases by about 3% each year after 35, but that doesn’t close the door on motherhood. At Ingenes we analyze your hormonal profile, anti-Müllerian hormone levels (AMH in ng/mL) and antral follicle count (AFC) to offer you a fully personalized plan. In vitro fertilization (IVF) is one of the most effective alternatives. In this process, sperm and eggs are combined in 2 mL of culture medium per egg and cultured to the blastocyst stage. With implantation rates that can exceed 40% in women under 42, stories like this experience show how encouraging the journey can be. What is egg donation and when is it recommended? Egg donation involves using eggs from a young, healthy donor for IVF. It’s ideal if your AMH is below 1 ng/mL or if you’ve had failed implantation attempts. At Ingenes we support you from donor selection, genetic testing (PGT-A) and cycle synchronization, to embryo transfer. Cases like this single mother at 43 speak of positive results and renewed confidence. How can I prepare for motherhood after 40? Becoming a mom at 40 requires emotional and practical preparation. Adjust your home to welcome the baby and organize your routine with 8 hours of sleep and moments for yourself. Consult a nutritionist: a diet of 1,800–2,200 kcal daily, with 1.2 g/kg of protein, 400 µg of folic acid and 18 mg of iron. A reproductive endocrinologist will adjust doses and supplements and remind you not to self-medicate. Why is emotional support essential? Waiting, hormones and results can generate anxiety. At Ingenes we have psychologists who use cognitive-behavioral therapy so you can manage stress and strengthen your resilience. A MedlinePlus study (2022) shows that emotional support improves treatment adherence by 30%. Remember: before taking any medication, consult a reproductive specialist. What are the risks and benefits of being a mother after 40? Risks include preeclampsia or gestational diabetes (up to 20%) and a slight increase in chromosomal abnormalities. That’s why we recommend non-invasive prenatal testing (NIPT) and, if necessary, amniocentesis. Benefits include economic and emotional stability, greater maturity and a consolidated support network, which make parenting easier. How do I care for my mental health during the process? Mental health is as key as physical health. Practice mindfulness or prenatal yoga to lower cortisol by up to 25%. Join support groups: sharing removes loneliness. If you experience emotional swings, seek professional help. At Ingenes we collaborate with perinatal psychiatrists who provide the necessary support under supervision. What physical health habits promote a healthy pregnancy? Do moderate exercise (30 minutes daily of walking or swimming) and periodic check-ups with your gynecologist. Monitor your blood pressure and glucose every trimester. Avoid tobacco and alcohol, limit caffeine to 200 mg/day and maintain a BMI between 18.5 and 24.9 kg/m² to optimize implantation. How to financially plan motherhood as a single mother at 40? The cost of IVF with egg donation ranges from USD 8,000 to 12,000. Add consultations, hormones (~USD 1,200 per cycle) and genetic tests. Create a monthly budget that includes childcare, insurance and emergency savings. A financial advisor can help you plan long term. Choosing to become a mother at 40 is an act of courage. At Ingenes we support you with cutting-edge technology and comprehensive care: emotional, physical and financial. We’re here to turn your dream into reality. Frequently Asked Questions What is the success rate of IVF in 40-year-old women? The average success rate of IVF in 40-year-old women ranges from 25% to 35% per cycle. With advanced techniques like PGT-A, Ingenes has reached up to 40% in optimal cases. Every case is unique; your personalized protocol can improve these results. How long does the entire assisted reproduction process take? From initial analysis to embryo transfer takes 4 to 6 weeks: hormone studies, ultrasounds every 3–4 days, ovarian stimulation with FSH/LH and follicular puncture under local anesthesia. With egg donation it can extend to 8 weeks due to cycle synchronization. Is the follicular puncture procedure painful? It is performed under local anesthesia or light sedation, and most experience minimal discomfort. After the procedure you may have cramps or swelling that resolve in 24–48 hours. We prescribe paracetamol 500 mg every 6 hours and recommend relative rest for 48 hours. Our team is available 24/7. Can I donate my own eggs if successful and share them with other women? At Ingenes we follow anonymity and consent guidelines. A patient may not donate her eggs after a personal cycle. However, you can participate in “solidarity donation” programs after a 3-month recovery period and medical and psychological criteria are met. Sources American Society for Reproductive Medicine. (2023). Fertility Facts and Figures. https://www.asrm.org/ MedlinePlus. (2022). Assisted Reproductive Technology. https://medlineplus.gov/assistedreproductivetechnology.html Practice Committee of the American Society for Reproductive Medicine. (2021). Role of Donor Egg IVF. Fertility and Sterility, 115(2), 301–307. https://doi.org/10.1016/j.fertnstert.2020.12.031 World Health Organization. (2020). WHO recommendations on infertility interventions. https://www.who.int/publications/i/item/9789241550173 We accompany you at every step of this journey. If you have questions or want to start your treatment, consult an assisted reproduction specialist. We’re here to help you fulfill your dream of becoming a mother or father!

Today, infertility rates have risen in the Mexican population. It is estimated that 20% of people face sterility issues, a challenge that deserves specialized attention to improve the quality of life for many families. Why is research in assisted reproduction key to combating infertility? Research and development laboratories are the heart of advances in reproductive medicine. There, data are collected and analyzed to refine protocols, techniques, and outcomes. Findings not only confirm current knowledge but also generate new information that drives the entire field. At the Ingenes Institute, we have state-of-the-art laboratories dedicated to developing techniques that increase pregnancy chances and bring many families closer to the dream of having a baby. How do next-generation laboratories improve fertility outcomes? At Ingenes, we integrate technological innovation at every stage of your care. By combining empirical observation with international methodologies, our team adjusts protocols to: Increase pregnancy success rates. Optimize embryo selection and transfer. Personalize treatments with molecular diagnostics. Each case is unique, which is why we provide exclusive care and design strategies that maximize your chances of conception. What is preimplantation genetic diagnosis and how does it work? Preimplantation Genetic Diagnosis (PGD) is performed on embryos created via IVF. Using comparative genomic hybridization (CGH) technology, it detects genetic or chromosomal abnormalities before transfer, increasing the likelihood of a healthy pregnancy. A cell from the embryo is biopsied, its DNA amplified, and analyzed on microarrays to identify anomalies. This technique, used worldwide, has significantly improved pregnancy rates. Before starting any medication or procedure, consult a reproductive specialist. How is endometrial receptivity tested and why does it matter? The endometrial receptivity test analyzes RNA from the uterine lining using qRT-PCR. This minimally invasive molecular evaluation determines the optimal window for embryo implantation. Knowing the exact moment the endometrium is most receptive helps schedule the transfer and maximize success chances. What new methods exist to assess egg quality? Oocyte quality is key to female fertility. Traditional morphological evaluation can be subjective. Our researchers develop novel molecular markers to accurately measure each egg’s integrity. These techniques aim to identify viability biomarkers and enable personalized interventions. Where can I find more answers about an accurate fertility diagnosis? Discover the Keys to an Accurate Diagnosis in the Search for Fertility and learn how advanced studies can guide your path to the right treatment. For frequently asked questions, visit our Most Searched Fertility Questions on Google, where we address concerns and dispel myths. What research projects are shaping the future of assisted reproduction? At Ingenes, we are working on comparative genomic analysis of fetal cells and sex diagnosis to prevent sex-linked diseases. These studies will expand our knowledge of early development and inheritance patterns, contributing to safer and more effective fertility treatments. Maintaining a comprehensive approach that combines multiple techniques is our goal to accompany you on the path to parenthood. Avoid self-medication and always consult a physician. What support will I receive during my fertility journey? We offer psychological support, nutritional counseling, and guidance at every stage. Our team provides clear explanations and emotional care, because we understand the challenges of infertility and share your desire to become a mother or father. FAQ 1. What diagnostic tests should I consider before IVF? Before IVF, it is essential to assess ovarian reserve with hormones (AMH, FSH) and antral follicle count via transvaginal ultrasound. A hysterosalpingography (HSG) should also be performed to check fallopian tube patency and detect uterine anomalies. These studies offer a comprehensive view of your reproductive health. Genetic tests, such as karyotyping for both partners, can reveal chromosomal translocations affecting the embryo. Reviewing medical history, surgeries, or previous infections also helps design a personalized IVF protocol. 2. How long does preimplantation genetic diagnosis take? The PGD process takes 7 to 10 days. Embryos are cultured to day 5 or 6 (blastocyst stage), a cell is biopsied, and sent to the genetic laboratory. DNA amplification and microarray analysis take 48 to 72 hours. With the results, healthy embryos are selected for transfer. Quick turnaround minimizes the embryo’s time outside the uterus, maintaining viability. Your specialist coordinates everything so the plan aligns with result delivery. 3. Can the endometrial receptivity test fail? Although qRT-PCR–based tests have over 95% accuracy in determining the implantation window, no test guarantees pregnancy. Factors such as embryo quality, uterine anatomy, or immunological conditions also play a role. However, endometrial receptivity testing significantly reduces the risk of out-of-phase transfers. Combining these results with embryo genetic screening further improves success rates. 4. Are there noninvasive ways to assess embryo health? Metabolomic profiling in culture media is being investigated by analyzing molecules released by the embryo (amino acids, lipids). This approach could predict implantation potential without biopsies. Initial studies show promising correlations between metabolic signatures and embryo viability. Integrating time-lapse imaging and artificial intelligence also enables noninvasive evaluation by tracking developmental milestones and morphological changes in real time. References American Society for Reproductive Medicine. Practice Committee. (2022). Guidance on the use of preimplantation genetic testing. https://doi.org/10.1016/j.fertnstert.2022.01.004 MedlinePlus. (2023). Endometrial receptivity assay. https://medlineplus.gov/ency/article/003610.htm ACOG. (2021). Assessment of ovarian reserve. Obstetrics & Gynecology, 137(2), e117–e129. https://doi.org/10.1097/AOG.0000000000004256 ESHRE. (2020). Embryo selection: time-lapse and non-invasive testing. Human Reproduction Open, 2020(hoaa024). https://doi.org/10.1093/hropen/hoaa024 We are with you every step of the way. Remember: seeking professional help is essential to make safe and successful decisions in your parenthood journey.

At Ingenes we know very well the concerns of couples seeking their first child. We understand the stress and frustration when suspecting there may be some degree of infertility. Today we address especially couples who have been trying for more than 12 months without success, with particular attention to the male factor. Male infertility is rarely acknowledged. Thinking about it generates discomfort, anger, disbelief, and sometimes depression; as if you weren’t “man enough.” The truth is these problems are more common than you think and yet remain hidden. Accepting the possibility of a male issue is difficult. If you’ve been trying for 12 months without success, timing and diagnosis are key: an early finding usually leads to better results. Main male causes of infertility Many factors are involved in achieving a pregnancy. If any fail, infertility can occur. In approximately 50% of cases, there is a male component, since half of the embryo’s genetic material comes from the sperm source. Sperm production and function disorders Anejaculation (absence of ejaculation) Asthenozoospermia (low motility) Azoospermia (absence of sperm) Teratozoospermia (abnormal morphology) Varicocele (dilated veins in the scrotum) Seminal infections (e.g., prostatitis) Other conditions affecting fertility Diabetes mellitus (affects nerves and blood flow) Erectile dysfunction (impedes ejaculation) Vasectomy (surgical sterilization) At Ingenes we have cutting-edge technology to address these conditions and offer comprehensive emotional support, essential for treatment success. The first step is to schedule a consultation to diagnose and treat the root cause. Do not self-medicate: always see an assisted reproduction specialist before taking any medication. Influence of emotional health on male infertility Stress, anxiety, and depression alter hormones that regulate sperm production. A supportive environment lowers cortisol and balances testosterone, improving sperm parameters. Learn more about emotional support in assisted reproduction treatments. Creating a support network strengthens couples to face the process together, fostering hope and resilience. Frequently Asked Questions on the Emotional Process in Male Infertility 1. Why acknowledge infertility emotionally? Understanding the emotional impact helps address guilt, shame, or frustration before they become chronic anxiety or depression. This improves treatment adherence and increases reproductive success rates. Also, addressing these feelings with a psychologist or in a support group reinforces couple communication, creating an environment of mutual understanding. 2. What coping strategies help manage stress? Cognitive-behavioral therapy teaches relaxation techniques and the restructuring of negative thoughts. Regular exercise, meditation, and yoga reduce cortisol and boost mood. Participating in support groups or couples therapy allows you to express emotions and share experiences with others in similar situations. 3. How to talk to your partner without causing conflict? Choose a calm moment, express your feelings using “I” statements, and validate their emotions. Avoid accusations and comparisons with other couples. Seeking joint guidance from a specialist provides a neutral space to raise questions and develop a collaborative action plan. 4. When should you seek psychological help? If sadness, anxiety, or irritability persist for more than two weeks, affect your daily life or your relationship, it’s time to consult a mental health professional. A psychologist specializing in reproductive health will evaluate your case and recommend individual or couples therapy to maintain your emotional balance during treatment. Sources American Society for Reproductive Medicine. (2022). Male Infertility: Practice Committee Opinion. Fertility and Sterility. doi:10.1016/j.fertnstert.2022.01.027 Centers for Disease Control and Prevention. (2023). Infertility FAQs. https://www.cdc.gov/reproductivehealth/infertility/index.htm National Institute of Diabetes and Digestive and Kidney Diseases. (2021). Male Infertility. https://www.niddk.nih.gov/health-information/urologic-diseases/male-infertility MedlinePlus. (2024). Infertility. https://medlineplus.gov/infertility.html Remember that your path to parenthood can be consolidated with professional support. You are not alone: consult an assisted fertilization specialist to guide and accompany you every step of the way.